Bariatric Surgery: Gastric Bypass vs. Sleeve Gastrectomy - What Really Matters
When you’re struggling with severe obesity, losing weight isn’t just about willpower. It’s about biology. And sometimes, your body needs a reset. That’s where bariatric surgery comes in. Of all the options, two procedures dominate: gastric bypass and sleeve gastrectomy. Both help you lose weight. But they do it in completely different ways. And that difference changes everything - from how much weight you lose, to how you feel years later, to what supplements you’ll be taking for the rest of your life.
How Each Surgery Works
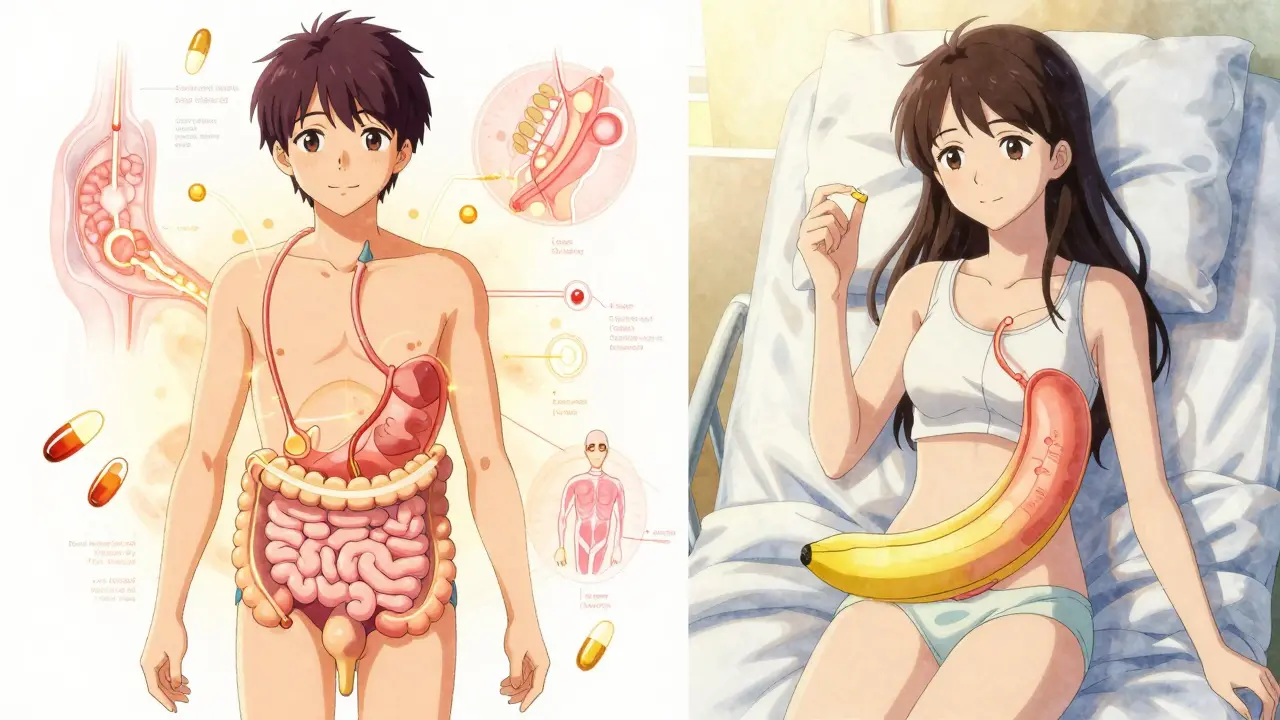
Gastric bypass, or Roux-en-Y gastric bypass, isn’t just about making your stomach smaller. It rewires your digestive system. Surgeons cut off the top part of your stomach to create a small pouch - about the size of a golf ball. Then, they connect that pouch directly to the middle part of your small intestine, skipping the rest of the stomach and the first section of the intestine. Food bypasses most of your digestive tract. That means fewer calories get absorbed. It also changes the hormones that tell your brain when you’re full.
Sleeve gastrectomy is simpler. About 80% of your stomach is removed. What’s left is a narrow tube - shaped like a banana - that holds just 2 to 5 ounces. That’s it. No rerouting. No bypassing. Just a smaller stomach that fills up faster. You still digest food the same way. But you can’t eat as much before you feel full.
The surgery time reflects the difference. Sleeve gastrectomy takes about 47 minutes on average. Gastric bypass? Around 68 minutes. That’s not just a difference in minutes - it’s a difference in complexity. And complexity affects risk.
Weight Loss: How Much and How Fast
If your goal is maximum weight loss, gastric bypass usually wins. Studies show people lose 57% of their excess weight with gastric bypass after five years. Sleeve gastrectomy? Around 49%. That gap might not sound huge, but for someone who weighs 300 pounds, it’s an extra 20 to 30 pounds of fat gone.
And the pace? Gastric bypass often delivers faster results. Many patients lose 60-80% of excess weight within the first year and a half. Sleeve patients lose 60-70% too - but it takes longer. Slower, steadier. Some people prefer that. Others want the quicker payoff.
Long-term data from a 2022 study of over 95,000 Medicare patients found that while gastric bypass led to more weight loss, it didn’t always mean better outcomes. Why? Because weight isn’t the only thing that matters.
Risks and Complications
Here’s where things get real. Both surgeries are safe when done by experienced teams. But they’re not equal in risk.
Gastric bypass carries a higher risk of death within five years. The same 2022 study found 5.67% of bypass patients died compared to 4.27% of sleeve patients. That’s a 32.8% lower risk of death with the sleeve. It also has higher rates of complications like internal hernias, bowel obstructions, and ulcers.
Sleeve gastrectomy has its own problems. The biggest? Revisions. About 3.2% more sleeve patients need another surgery within five years. Why? Weight regain. Or severe acid reflux. Or the sleeve stretches out. That’s why some surgeons now recommend endoscopic procedures - like tightening the sleeve with sutures - to fix weight regain without open surgery.
Then there’s dumping syndrome. It happens in 50-70% of gastric bypass patients. Eat sugar or carbs? Your stomach dumps them too fast into your intestine. You get dizzy, sweaty, nauseous, maybe even faint. It’s scary. But it also teaches you to avoid junk food. For some, it’s a lifesaver. For others, it’s a daily nuisance.
Sleeve patients rarely get dumping syndrome. But they’re more likely to develop or worsen GERD - acid reflux. That’s because the surgery changes pressure in the stomach. Some patients end up needing anti-reflux meds long-term.
Nutrition and Lifelong Changes
This is where most people get caught off guard. After surgery, you don’t just eat less. You absorb less. And that changes everything.
Gastric bypass patients need lifelong supplements: vitamin B12, iron, calcium, vitamin D, and folate. Blood tests every six months aren’t optional - they’re life-saving. Without them, you risk anemia, nerve damage, or osteoporosis. The malabsorption that helps you lose weight also steals nutrients from your body.
Sleeve gastrectomy patients need supplements too - but far fewer. Annual blood tests are usually enough. That’s because the stomach and intestines still work the same way. You just have less space to eat. Fewer complications. Fewer pills. Fewer doctor visits.
And diet? Sleeve patients often find it easier to eat normally. You can still enjoy most foods - just in smaller portions. Gastric bypass patients have to be more careful. Too much sugar? Dumping. Too much fat? Nausea. Too much fiber? Blockage. It’s not that you can’t eat anything - it’s that your body reacts differently. And you have to learn those rules.
Cost, Insurance, and Access
Cost matters. A lot.
As of late 2024, sleeve gastrectomy costs about 25% less than gastric bypass. Out-of-pocket? Around $14,500 for sleeve versus $19,300 for bypass - assuming insurance covers 80%. That’s not just money. It’s stress. It’s whether you can afford the follow-up care.
Insurance rules are tightening. Many insurers now require a BMI of 45 or higher for coverage, not just 35. Some, like UnitedHealthcare, updated their guidelines in January 2024. Others still follow the NIH standard: BMI ≥40, or ≥35 with conditions like diabetes or high blood pressure.
Both procedures require the same prep: six months of documented weight management, a psychological evaluation, and medical clearance. But after surgery, gastric bypass demands more ongoing care - more labs, more visits, more vigilance.

Why Sleeve Gastrectomy Is Now the Most Popular
In 2010, sleeve gastrectomy made up less than 10% of bariatric surgeries. Today? Over 60%. In 2022, out of nearly 287,000 bariatric procedures in the U.S., 63.2% were sleeves. Only 27.4% were bypasses.
Why? Because patients want less risk, less hassle, and faster recovery. Surgeons prefer it too - it’s easier to teach, faster to perform, and has fewer long-term complications. The data supports it: lower death rates, fewer nutritional emergencies, fewer hospital readmissions.
But here’s the twist: gastric bypass still works better for people with type 2 diabetes. Studies show higher remission rates. The hormonal changes it triggers - especially in the gut - help insulin work better. That’s why some doctors still recommend bypass for diabetic patients, even if they’re not the highest risk.
Which One Is Right for You?
There’s no universal answer. But here’s how to think about it:
- Choose gastric bypass if: You have type 2 diabetes, want the most weight loss possible, and are ready for lifelong monitoring and strict dietary rules.
- Choose sleeve gastrectomy if: You want a simpler surgery, fewer supplements, lower risk of death, and are okay with slower weight loss and a small chance of needing a revision later.
Most people who choose sleeve don’t regret it. Most who choose bypass don’t regret it either - but they often say, "I wish I’d known how strict the diet would be."
The truth? Both surgeries save lives. Both reduce diabetes, high blood pressure, and sleep apnea. Both cut cancer risk. Both give you back your energy. But one gives you more weight loss. The other gives you fewer problems down the road.
It’s not about which is better. It’s about which is better for you.
Can I switch from sleeve to gastric bypass later?
Yes, but it’s not simple. A revision from sleeve to bypass is a major surgery with higher risks than the original procedure. It’s usually only done if you’ve regained significant weight, developed severe GERD, or have uncontrolled diabetes. Surgeons will evaluate your health, nutritional status, and reasons for revision before approving it.
Which surgery has fewer long-term side effects?
Sleeve gastrectomy generally has fewer long-term side effects. It doesn’t alter nutrient absorption like gastric bypass does, so you’re less likely to develop deficiencies in iron, B12, or calcium. It also has lower rates of internal hernias, bowel obstructions, and ulcers. However, sleeve patients are more likely to need a second surgery for weight regain or reflux.
Do I need to take supplements forever after either surgery?
Yes, but the amount differs. After gastric bypass, you’ll need lifelong daily supplements - including B12 injections, iron, calcium, vitamin D, and folate. After sleeve gastrectomy, you’ll still need a daily multivitamin and calcium, but fewer additional supplements. Blood tests are recommended annually for sleeve patients and every six months for bypass patients to catch deficiencies early.
Is one surgery better for people with type 2 diabetes?
Gastric bypass has consistently shown higher rates of type 2 diabetes remission - often over 80% in studies. This is because the bypass changes gut hormones that regulate blood sugar, not just because you eat less. Sleeve gastrectomy also improves diabetes, but typically at a lower rate - around 60-70%. For diabetic patients, bypass is often the preferred choice if they can handle the long-term nutritional demands.
How long is recovery after each surgery?
Recovery time is similar: most people go home the same day or the next day. You’ll need 2-4 weeks to return to normal activities. Sleeve patients often feel better sooner because the surgery is less invasive. Gastric bypass patients may feel more fatigued in the first few weeks due to the body adjusting to the new digestive path. Both require a liquid-to-solid diet progression over several weeks.

Sam Pearlman
February 16, 2026 AT 19:48Adam Short
February 16, 2026 AT 21:17