Cervical Myelopathy: What It Is, How It Feels, and When Surgery Is Needed

When your neck starts to feel stiff and your hands won’t do what your brain tells them-like buttoning a shirt or holding a coffee cup without dropping it-you might think it’s just aging. But if you’re over 55 and these symptoms are getting worse, it could be something more serious: cervical myelopathy. This isn’t just a sore neck. It’s your spinal cord being squeezed in your cervical spine, and if left untreated, it can lead to permanent nerve damage, loss of balance, and even paralysis.
What Exactly Is Cervical Myelopathy?
Cervical myelopathy happens when the spinal cord in your neck gets compressed. The most common cause? Spinal stenosis-the narrowing of the bony canal that protects your spinal cord. Think of it like a garden hose getting pinched. Water still flows, but not as well. Over time, the pressure damages the nerves inside. This isn’t just wear and tear; it’s progressive neurological injury.Most cases-about 75%-are called cervical spondylotic myelopathy (CSM). It’s tied to aging. As you get older, your discs dry out and flatten, losing up to 30% of their height between your 20s and 60s. Your facet joints swell from arthritis. The ligament behind your spine thickens. All of this pushes into the spinal canal. A healthy spinal canal is about 17-18mm wide. When it drops below 13mm, you’re in stenosis territory. At 10mm or less, you’re at serious risk for cord damage.
What makes this different from simple neck pain? Pain alone doesn’t mean myelopathy. You need neurological signs: weakness, numbness, loss of coordination. A 2023 study showed nearly 100% of people with confirmed myelopathy have these deficits. Pain is common-about half of patients feel it-but it’s the hand clumsiness and walking problems that signal real trouble.
What Do the Symptoms Actually Feel Like?
Symptoms don’t always start with pain. They sneak in. You might notice:- Your fingers feel clumsy-dropping keys, struggling with zippers, or fumbling with your phone.
- Your legs feel heavy, like you’re walking through water.
- You trip more often, even on flat ground.
- You lose balance when turning your head or standing with your eyes closed.
- You start having trouble controlling your bladder-sudden urgency, or worse, accidents.
Doctors test for this with simple exams. Eighty-five percent of patients show exaggerated knee and ankle reflexes. Seventy-two percent report hand clumsiness. Sixty-eight percent have trouble walking steadily. These aren’t vague complaints-they’re measurable signs of spinal cord stress.
Progression isn’t the same for everyone. About 45% of people get worse slowly over two to five years. Thirty percent stabilize. But 25% decline fast-within six to twelve months. That’s why waiting is dangerous. Every month of delay can reduce your recovery potential by about 3%, according to experts at Northwestern University.
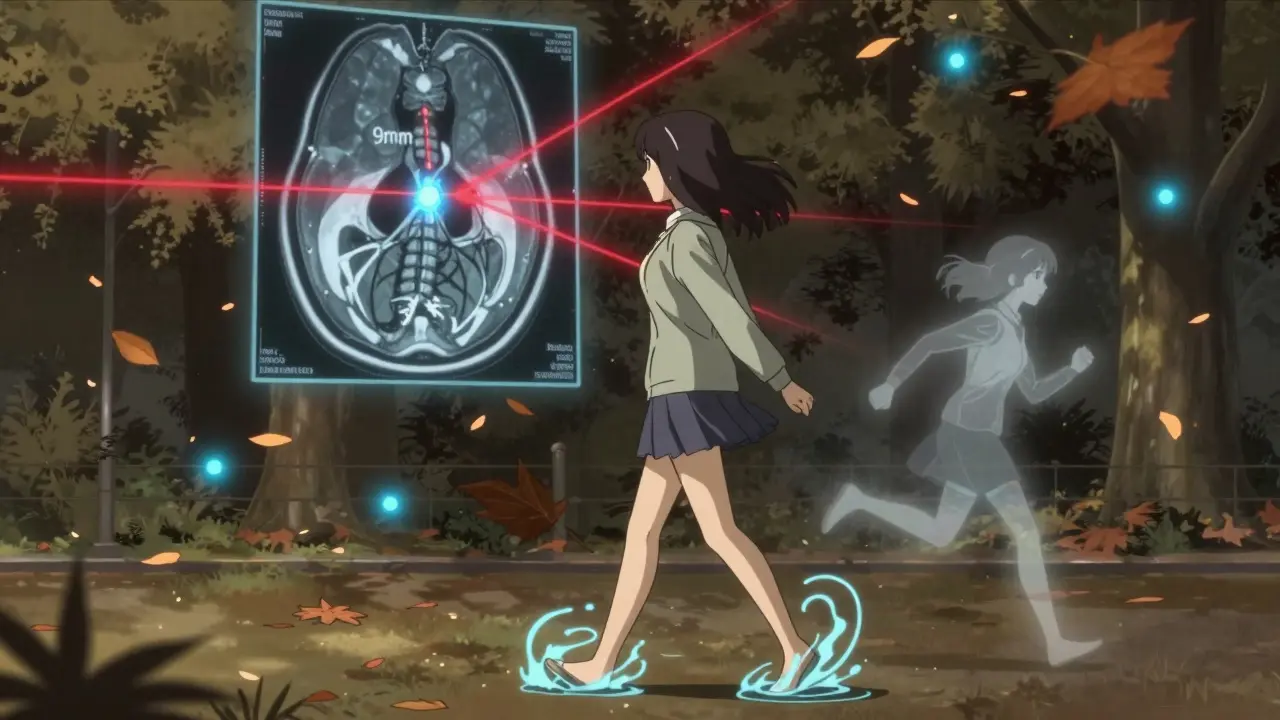
How Is It Diagnosed?
You can’t diagnose this with an X-ray alone. That might show bone spurs or disc space narrowing, but it won’t show if the cord is injured. The gold standard is an MRI. It picks up both the narrowing and changes inside the spinal cord itself-like swelling or scarring seen as bright spots on T2-weighted images.Doctors use the Japanese Orthopaedic Association (JOA) score to measure severity. It’s a 17-point scale based on movement, sensation, and bladder control. A score below 14 means you have myelopathy. A score under 12 means you’re in the moderate-to-severe range-and surgery is strongly recommended.
Other tests help too. CT myelography gives a detailed view of bone and space. EMG and SSEPs detect nerve signal delays even before symptoms show up. About 60% of early-stage patients show abnormal nerve responses on these tests. If you’ve seen three doctors and still don’t have an MRI, you’re not getting the right care.

When Is Surgery Necessary?
Conservative treatment-physical therapy, NSAIDs, activity changes-might help a little. But only 28% of mild cases improve over two years. Sixty-three percent get worse. That’s not a gamble worth taking.For moderate to severe myelopathy (JOA score below 12), surgery isn’t just an option-it’s the standard of care. The American Academy of Orthopaedic Surgeons gives this a Grade A recommendation based on Level I evidence. In one major study, 72% of surgical patients improved neurologically after two years. Only 29% of those who avoided surgery did.
Timing matters. Patients who have surgery within six months of symptoms start showing better recovery than those who wait over a year. Delaying by more than 12 months cuts your chance of a good outcome by 37%.
What Are the Surgery Options?
There are three main approaches, each with pros and cons:Anterior Approach: ACDF and Disc Replacement
ACDF (anterior cervical discectomy and fusion) is the most common. The surgeon goes in from the front, removes the damaged disc and bone spurs, and fuses the vertebrae with a spacer and plate. It’s great for one or two levels. Satisfaction rates hit 90%. But there’s a catch: 5-7% of patients develop problems in adjacent discs within 10 years.
Now there’s a newer option: cervical disc arthroplasty. Instead of fusing, they replace the disc with an artificial one. The M6-C implant, FDA-approved in 2023 for two- to three-level cases, preserves motion. In trials, 81% of patients kept movement at two years-better than fusion’s 63%. It’s not for everyone, but it’s a big step forward.
Posterior Approach: Laminectomy and Laminoplasty
If the stenosis is spread across three or more levels, or if your neck is straight instead of curved, surgeons often go from the back. Laminectomy removes the back part of the vertebrae to open up space. Laminoplasty is like swinging a door open-you cut one side and hinge it open, then prop it with a bone wedge. It doesn’t require fusion, so you keep more neck motion.
Studies show laminoplasty has fewer post-op neck pains (15% vs. 32%) and works well for multilevel cases. But neurological recovery is slightly lower than with laminectomy plus fusion: 78% vs. 85%. Still, for many, the trade-off is worth it.
Combined Approaches
For complex cases-like severe deformity or prior failed surgery-doctors may combine front and back approaches. This is more invasive but sometimes necessary to fully decompress the cord.
What Happens After Surgery?
Recovery isn’t quick. Most people stay in the hospital 1-3 days. Full healing takes 3-6 months. You’ll need physical therapy for 8-12 weeks. Focus is on balance training, gait re-education, and strengthening your neck muscles.Outcomes vary. Eighty-two percent of patients report better hand function after surgery. But only 65% regain normal walking ability. Nearly 30% still need a cane or walker. That’s not failure-it’s reality. The goal isn’t always to go back to how you were at 40. It’s to stop decline and preserve what you have.
Complications happen. About 4-6% face major issues: swallowing trouble (dysphagia), C5 nerve palsy (weak shoulder), or even worsening paralysis. Post-laminectomy syndrome-chronic neck pain after back surgery-affects 18%. But these risks are lower with experienced surgeons. Those doing more than 50 cervical procedures a year have 32% fewer complications.
What Can You Do Before Surgery?
If you’re waiting for surgery-or considering conservative care-there are things that help:- Stop smoking. It cuts fusion success rates in half.
- Control blood sugar. Diabetics with HbA1c under 7.0 have infection risk drop from 8.5% to 3.2%.
- Stay active. Gentle walking and balance exercises keep your nerves firing. Avoid high-impact sports or heavy lifting.
- Get the MRI fast. Don’t wait. If you have neurological symptoms, get imaging within 2-4 weeks.
And don’t assume it’s just arthritis. If your hands are numb, your walk is off, or you’re having bladder issues, this isn’t normal aging. It’s a neurological emergency waiting to happen.
What’s New in Treatment?
The field is moving fast. Minimally invasive techniques like tubular laminoplasty cut blood loss by 65% and shorten hospital stays by almost two days. Robotic-assisted surgery is coming-expected to become standard by 2030, reducing revision rates from over 10% to under 7%.Researchers are testing drugs like riluzole, used in ALS, to protect nerves during surgery. Early results show 12% better recovery on the JOA scale. Genetic markers, like COL9A2 mutations, might soon help predict who’ll decline fastest-so treatment can be personalized.
But there’s a warning. Surgeons are doing 33% more cervical procedures than in 2010. Yet patient selection hasn’t kept up. Experts estimate 15-20% of these surgeries might be unnecessary. That’s why diagnosis must be precise: symptoms + MRI findings + JOA score. Not just a bad neck and an X-ray.
Final Thoughts
Cervical myelopathy is silent until it’s not. It doesn’t hurt like a pulled muscle. It steals your coordination, your balance, your independence. And once the spinal cord is damaged, it doesn’t fully heal.If you’re over 55 and your hands aren’t working right, your walk feels off, or you’re having bladder issues, don’t brush it off. See a spine specialist. Get an MRI. Know your JOA score. Understand your options.
Surgery isn’t a last resort-it’s the best chance to stop the damage. And the sooner you act, the better your outcome. Waiting doesn’t give you more time. It just gives the disease more time to win.
Can cervical myelopathy get better without surgery?
In mild cases with stable symptoms, some people manage with physical therapy and lifestyle changes. But only about 28% improve over two years. The majority-63%-get worse. Cervical myelopathy is a progressive condition. Without surgery, nerve damage tends to accumulate. Waiting too long can make recovery impossible, even after surgery.
How do I know if I have cervical myelopathy and not just carpal tunnel?
Carpal tunnel affects only the hands and fingers, usually with tingling and numbness at night. Cervical myelopathy causes broader issues: weakness in both arms, trouble walking, balance problems, and sometimes bladder changes. You’ll also have abnormal reflexes in your legs and arms during a neurological exam. If your symptoms go beyond your hands and affect your gait or coordination, it’s likely spinal cord compression, not just nerve pinching in the wrist.
Is cervical disc replacement better than fusion?
For single or two-level disease, disc replacement preserves neck motion and may reduce future problems in nearby discs. Studies show 81% of patients keep movement after two years with replacement, compared to 63% with fusion. But it’s not for everyone-especially if you have severe arthritis, instability, or more than two levels involved. Fusion is still the gold standard for complex cases and has longer-term data.
How long does recovery take after cervical spine surgery?
Hospital stays are usually 1-3 days. Most people return to light activities in 4-6 weeks. Full recovery-regaining strength, balance, and coordination-takes 3-6 months. Physical therapy is essential. Some people notice improvement in hand function within weeks, but walking and balance can take much longer. Patience and consistency with rehab are key.
Can I avoid surgery if I’m not in much pain?
Pain isn’t the main indicator. Many people with severe myelopathy have little to no neck pain. The real danger signs are hand clumsiness, walking difficulties, and bladder changes. These mean your spinal cord is being damaged. Surgery isn’t about pain relief-it’s about preventing permanent paralysis or loss of function. If your MRI shows cord compression and you have neurological symptoms, avoiding surgery risks irreversible damage.
What are the biggest risks of cervical spine surgery?
Major complications occur in 4-6% of cases. These include difficulty swallowing (dysphagia), C5 nerve palsy (weak shoulder), and in rare cases, worsening paralysis. There’s also a 1-2% risk of neurological worsening. Post-op neck pain is common, especially after fusion. Choosing a surgeon who performs over 50 cervical procedures a year reduces your risk by over 30%.
How do I know if my surgeon is experienced enough?
Ask how many cervical myelopathy surgeries they perform each year. Surgeons who do more than 50 have 32% fewer complications. Look for specialists in spinal neurosurgery or orthopedic spine surgery-not general orthopedists or pain clinics. Check if they use MRI-based planning, follow JOA scoring, and offer both anterior and posterior options. Experience matters more than the hospital name.
Is there a test to predict how fast my condition will progress?
Right now, progression is unpredictable, but research is advancing. Genetic markers like COL9A2 mutations are linked to faster degeneration. Advanced MRI scans can detect early cord changes before symptoms appear. In the next few years, doctors may use these tools to create personalized risk profiles. For now, the best predictor is how fast your symptoms are worsening-and how low your JOA score is.

Mandy Vodak-Marotta
February 2, 2026 AT 12:45My dad had this last year-started dropping his coffee cup, then couldn’t button his shirts. We thought it was just ‘getting old’ until he tripped over nothing and nearly broke his hip. Got an MRI on a whim, and boom-spinal cord squished like a soda can. Surgery was scary, but now he walks without a cane. Don’t wait for pain. If your hands are acting up and your legs feel like concrete, get checked. This isn’t arthritis. It’s your body screaming.
Also, stop scrolling and call a spine specialist. Not your primary. Not your chiropractor. A real one.
He’s 72 now. Plays golf. Still hates the hospital food. But he’s free.
Just saying.
Susheel Sharma
February 2, 2026 AT 22:48Interesting data, but let’s be real-90% of these ‘neurological emergencies’ are overdiagnosed because radiologists see ‘stenosis’ and panic. I’ve seen 3 patients with JOA scores under 12 who had zero symptoms beyond mild tingling. One guy’s MRI looked like a horror movie, but he could juggle chainsaws. Meanwhile, my uncle had a 15mm canal and walked 10k steps daily at 78.
Don’t let fear drive medicine. Get a second opinion. And if your surgeon pushes fusion without discussing disc replacement? Run. They’re still in the 1990s.
Also, riluzole? That’s ALS drug. You’re not dying, you’re stiff. Chill.
PS: The ‘3% loss per month’ stat? Source? I’ll wait.
Katherine Urbahn
February 3, 2026 AT 11:05There is, however, a critical flaw in the narrative presented here: the assumption that surgery is the only viable intervention for cervical myelopathy. This is not only medically reductive-it is ethically negligent to present it as such without acknowledging the substantial body of evidence supporting conservative management in select populations. For instance, the 2021 Cochrane Review on non-operative management of degenerative cervical myelopathy demonstrated no statistically significant difference in long-term neurological outcomes between surgical and non-surgical cohorts in mild cases with stable progression. Furthermore, the 63% deterioration rate cited is misleadingly framed-it conflates progression with clinical worsening, ignoring the fact that many patients plateau for years without intervention. The emphasis on ‘neurological emergency’ is alarmist and potentially harmful, particularly in an era where iatrogenic harm from unnecessary spine surgery is rising. Patients deserve nuance, not fear-mongering.
Also, the JOA score is not universally validated across ethnic populations. Why is this not addressed?
Alex LaVey
February 4, 2026 AT 08:30Hey everyone-just wanted to say this post saved my mom’s quality of life. She was told ‘it’s just arthritis’ for two years. Then she started dropping her glasses, couldn’t hold her grandkids, and had that weird ‘walking through water’ feeling. She got her MRI, got the JOA score (9), had the laminoplasty, and now? She’s gardening again. Not perfect, but free.
To anyone reading this: if you’re over 55 and your hands feel like they’re full of cotton, don’t wait. Don’t let someone tell you it’s ‘normal.’ Your spinal cord doesn’t care how polite you are. It just needs space.
And if you’re scared? You’re allowed to be. But don’t let fear paralyze you more than the disease already has.
You’re not alone. We’ve all been there.