Diverticulitis: Understanding Inflamed Pouches and Modern Treatment Options
What Exactly Is Diverticulitis?
Diverticulitis happens when small pouches in your colon-called diverticula-get inflamed or infected. These pouches form when weak spots in the colon wall give way under pressure, usually from constipation or a low-fiber diet. They’re not rare. About 58% of people over 60 have them, though most never know it. Only about 1 in 4 of those people will ever develop inflammation, which is diverticulitis.
The pain is often sharp and localized in the lower left side of your belly. It doesn’t come and go like IBS. It stays. You might also have a fever over 38°C, feel nauseous, or notice changes in bowel habits. Some people mistake it for appendicitis, especially if they’re Asian, since right-sided diverticulitis is more common in those populations. The key difference? Diverticulitis usually brings a fever and elevated white blood cell count-signs your body is fighting infection.
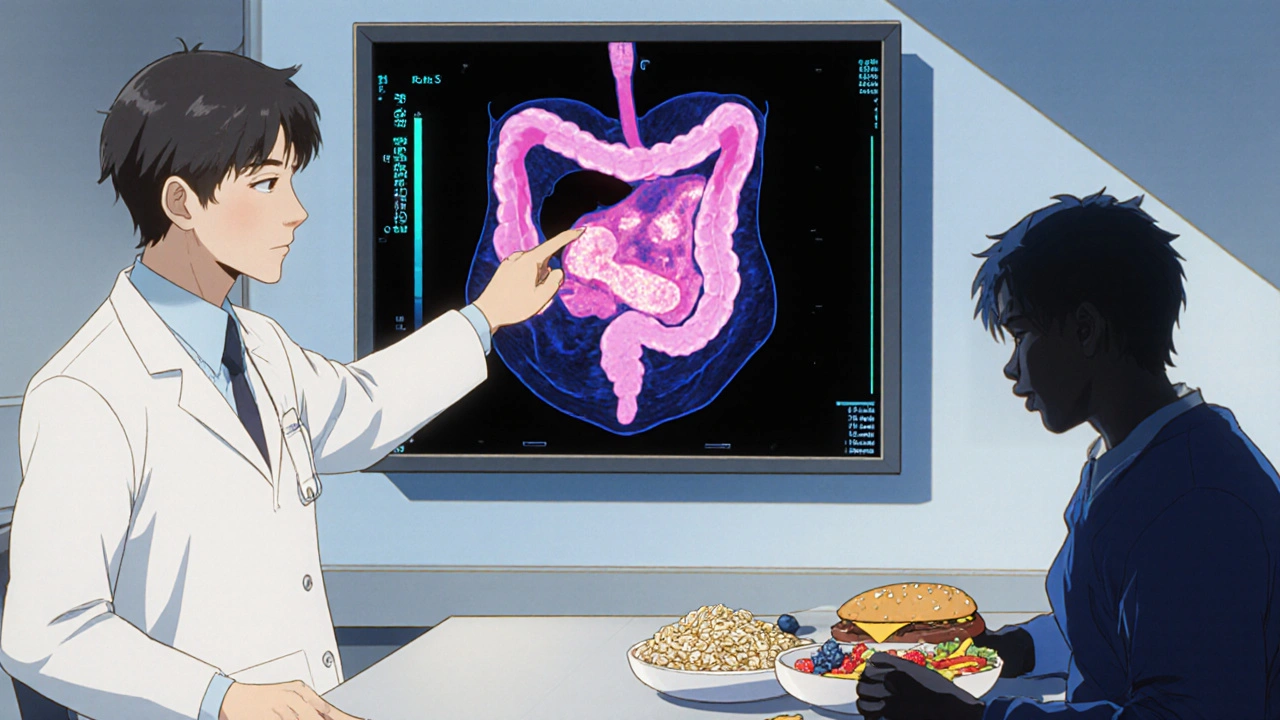
How Is It Diagnosed?
Doctors don’t just guess anymore. A CT scan is the gold standard. It shows the inflamed pouches, any abscesses, and whether there’s a perforation. You might think an ultrasound or blood test is enough, but those miss up to 25% of cases. Blood tests can show infection (white blood cells above 11,000), and physical exams reveal tenderness when pressing on the lower left abdomen. But only a CT scan confirms it and tells you how serious it is.
The Hinchey scale grades severity:
- Stage Ia: Small abscess near the colon
- Stage Ib: Larger abscess or spread to nearby tissue
- Stage II: Abscess in the pelvis
- Stage III: Pus in the abdominal cavity
- Stage IV: Fecal leakage into the belly-this is an emergency
Most people (70-80%) fall into Stage I. That’s good news. It means most cases can be treated without surgery.
When Do You Need Antibiotics?
This is where things changed. Ten years ago, every case got antibiotics. Now? Not always. The 2021 DIVERT trial showed that for mild, uncomplicated diverticulitis, antibiotics didn’t speed up recovery. Patients on just fluids and rest got better just as fast as those on amoxicillin-clavulanate.
So when do you still need them? If you have a fever above 38.5°C, a very high white blood cell count, or signs of spreading infection, yes-antibiotics matter. For others, doctors are skipping them. It cuts down on side effects, reduces antibiotic resistance, and saves money. The American Gastroenterological Association updated its guidelines in 2023 to reflect this shift.
Common antibiotics used when needed: amoxicillin-clavulanate for mild cases, piperacillin-tazobactam for hospitalized patients. Avoid NSAIDs like ibuprofen-they raise the risk of a hole in the colon.
What Should You Eat During and After an Attack?
For the first 48 to 72 hours, stick to clear liquids: water, broth, gelatin, electrolyte drinks. No solids. Your colon needs rest. After that, move to low-fiber foods-white rice, eggs, skinless chicken, canned vegetables without seeds. Keep it simple.
Once you’re better, the real work begins: fiber. A high-fiber diet isn’t just helpful-it’s your best defense against another attack. The goal? At least 30 grams a day. That’s whole grains, beans, lentils, berries, apples, broccoli, and oats. One patient reported going 27 months without another flare after hitting 35g daily.
And here’s the myth busted: nuts, seeds, and popcorn don’t cause diverticulitis. A 18-year study of 47,000 women found no link. You can eat them. In fact, they’re great sources of fiber.
What About Surgery?
Surgery used to be recommended after three attacks. Now, it’s after two-especially if one required hospitalization. Why? Because between attacks, many people live with constant discomfort, bloating, or fear of the next flare. One study found 40% of patients had major lifestyle restrictions even when not actively sick.
Two main procedures:
- Laparoscopic lavage: Clean out the infection without removing part of the colon. Works well for Stage III if the leak is contained.
- Resection: Remove the damaged section of colon (usually the sigmoid). This is the most common long-term fix.
The 2022 SCANDIV trial showed laparoscopic lavage had an 82% success rate for contained perforations. But if you’re young and healthy, resection gives you the best chance of never having another attack.
After surgery, you’ll need a colonoscopy 6 to 8 weeks later to rule out colon cancer. About 1.3% of people over 50 with diverticulitis turn out to have hidden cancer.
Who’s at Risk-and What You Can Control
Age is the biggest factor. But younger people are getting it more. In 2000, only 14% of hospitalizations were in people under 44. Now it’s 22%. Why? Obesity, smoking, and sitting too much.
- Obesity (BMI over 30) doubles your risk
- Smokers are 2.7 times more likely to get it
- People who exercise less than 2 hours a week have a 38% higher chance
It’s not just about diet anymore. Movement matters. Stress might play a role too-though that’s still being studied. The gut-brain connection is real, and chronic stress can slow digestion, increasing pressure in the colon.

New Treatments on the Horizon
There’s exciting progress beyond antibiotics and surgery. In 2023, the FDA approved mesalazine (Pentasa®) for maintenance therapy. In the DIVA-2 trial, it cut recurrence by 31% over 12 months compared to placebo. It’s not a cure, but it’s a tool to keep attacks away.
AI is stepping in too. Mayo Clinic’s algorithm uses CT scans, lab results, and patient history to predict who’s likely to have another flare. It’s 83% accurate. That means doctors can now tailor follow-up care-not just guess.
And then there’s the microbiome. Researchers found patients with diverticulitis have 37% less Faecalibacterium prausnitzii, a good gut bacterium that calms inflammation. Future treatments might include targeted probiotics or fecal transplants. A $4.2 million NIDDK grant is funding this research right now.
What to Do If You Think You Have It
Don’t wait. If you have sudden, severe pain in your lower left abdomen, fever, or vomiting, go to urgent care or the ER. Don’t try to tough it out. Delayed diagnosis leads to complications.
Keep a symptom journal: when the pain started, what you ate, whether you had a fever, how you felt after. This helps your doctor spot patterns.
After recovery, schedule a follow-up. Get a colonoscopy if you’re over 50. Start eating more fiber. Walk daily. Quit smoking if you smoke. These aren’t just "good ideas." They’re your best insurance against a second attack.
Living With Diverticulitis
Most people who get diverticulitis go on to live normal lives. The key is prevention. You don’t need to be perfect. Just consistent. A high-fiber diet, regular movement, and avoiding smoking do more than any pill or surgery.
Patients on Reddit say it best: "The pain feels like being stabbed with hot knives." But they also say: "After I started eating beans every day, I haven’t had a flare in two years."
It’s not about fear. It’s about awareness. You can’t control your age, but you can control your plate, your steps, and your choices. And that’s where real power lies.

Gerald Cheruiyot
November 19, 2025 AT 17:50Michael Fessler
November 20, 2025 AT 01:43daniel lopez
November 20, 2025 AT 14:58Nosipho Mbambo
November 20, 2025 AT 18:55Katie Magnus
November 21, 2025 AT 00:28King Over
November 21, 2025 AT 07:18Johannah Lavin
November 23, 2025 AT 00:24Ravinder Singh
November 24, 2025 AT 11:35Russ Bergeman
November 24, 2025 AT 17:02Dana Oralkhan
November 26, 2025 AT 07:54Jeremy Samuel
November 26, 2025 AT 23:55Destiny Annamaria
November 27, 2025 AT 15:50Ron and Gill Day
November 28, 2025 AT 22:52Alyssa Torres
November 30, 2025 AT 22:44