Fertility Preservation Options Before Chemotherapy: What You Need to Know
Why Fertility Preservation Matters Before Chemotherapy
Chemotherapy doesn’t just fight cancer-it can also stop your body from having children later. For many people, especially those under 40, the idea of losing the chance to have biological children is as devastating as the cancer diagnosis itself. About 80% of common chemotherapy drugs, like those used for breast cancer or lymphoma, carry a high risk of damaging ovaries or testes. This damage can lead to early menopause in women or low sperm counts in men, sometimes permanently. The good news? There are proven ways to protect your fertility before treatment starts. But time is tight. If you wait too long, the window closes fast.
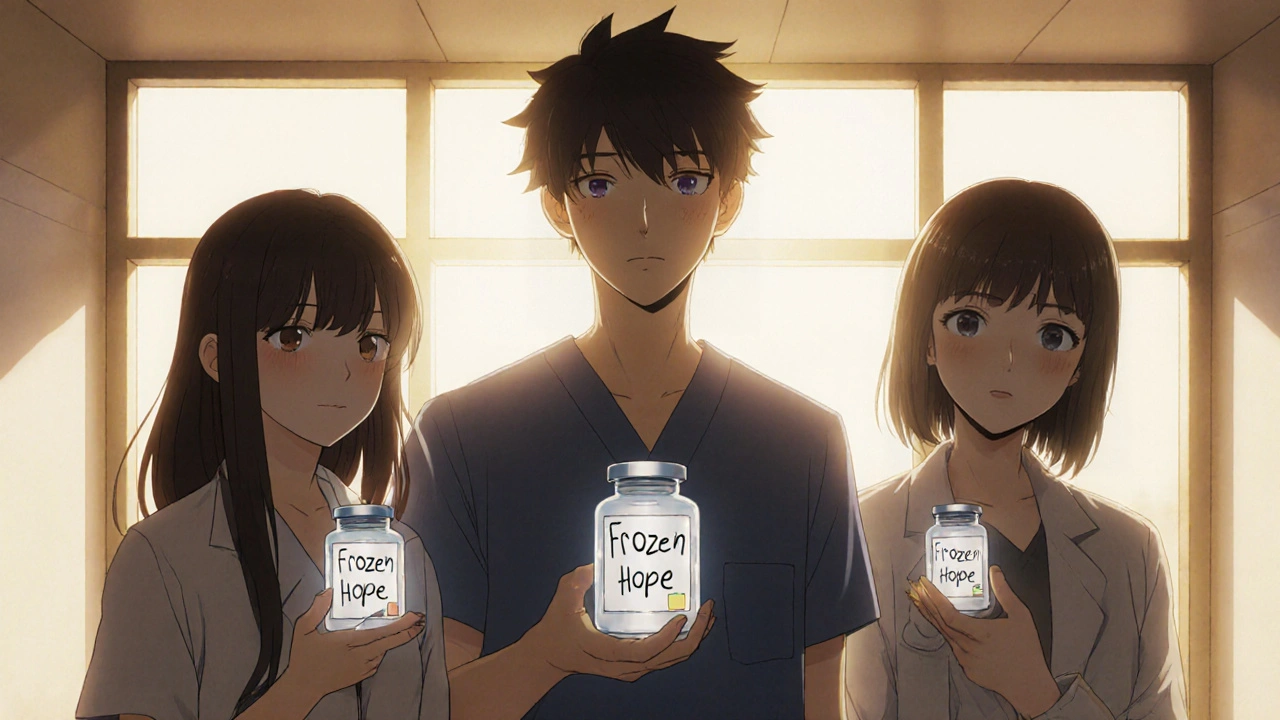
What Options Are Actually Available?
There are six main methods used today, each with different requirements, success rates, and timelines. Not all work for everyone, and some depend on your cancer type, age, and how quickly treatment must begin.
- Embryo cryopreservation - This is the most established option. Eggs are collected after 10-14 days of hormone injections, fertilized with sperm (from a partner or donor), and frozen as embryos. Success rates are highest here: 50-60% live birth rate per transfer for women under 35. But it requires sperm, which can be a barrier for single women or those not ready to choose a donor.
- Oocyte cryopreservation (egg freezing) - Same process as embryo freezing, but the eggs are frozen unfertilized. This gives you more control over future decisions. Pregnancy rates are slightly lower-4-6% per frozen egg-but you don’t need sperm right away. Most women need to freeze 15-20 eggs to have a decent chance of one baby later.
- Ovarian tissue cryopreservation - This is the only option for girls who haven’t reached puberty or women who can’t delay treatment. A small piece of ovarian tissue is removed through a quick laparoscopic surgery, frozen, and stored. Later, it can be re-implanted to restore hormone function and fertility. Around 200+ babies have been born this way worldwide. It’s still considered experimental by the FDA, but it’s widely used in Europe and increasingly in the U.S.
- Ovarian suppression with GnRHa - This isn’t a way to store eggs or sperm. Instead, monthly injections (like goserelin) temporarily shut down ovarian function during chemo. Studies show it reduces the risk of early menopause by 15-20%. It’s not a guarantee, but it’s low-risk and can be done quickly. Side effects? Hot flashes, night sweats, and mood swings-similar to menopause. Some women stop taking it because it’s too uncomfortable.
- Ovarian transposition - For women getting pelvic radiation, surgeons can move the ovaries out of the radiation field. This doesn’t help with chemo damage, but it can protect against radiation. It’s a one-time surgery and often done at the same time as other procedures.
- Sperm banking - For men, this is simple and effective. After 2-3 days of abstinence, semen is collected and frozen. Post-thaw motility rates are 40-60%. It’s fast, cheap, and doesn’t delay treatment. Even one sample can be enough for future IVF.
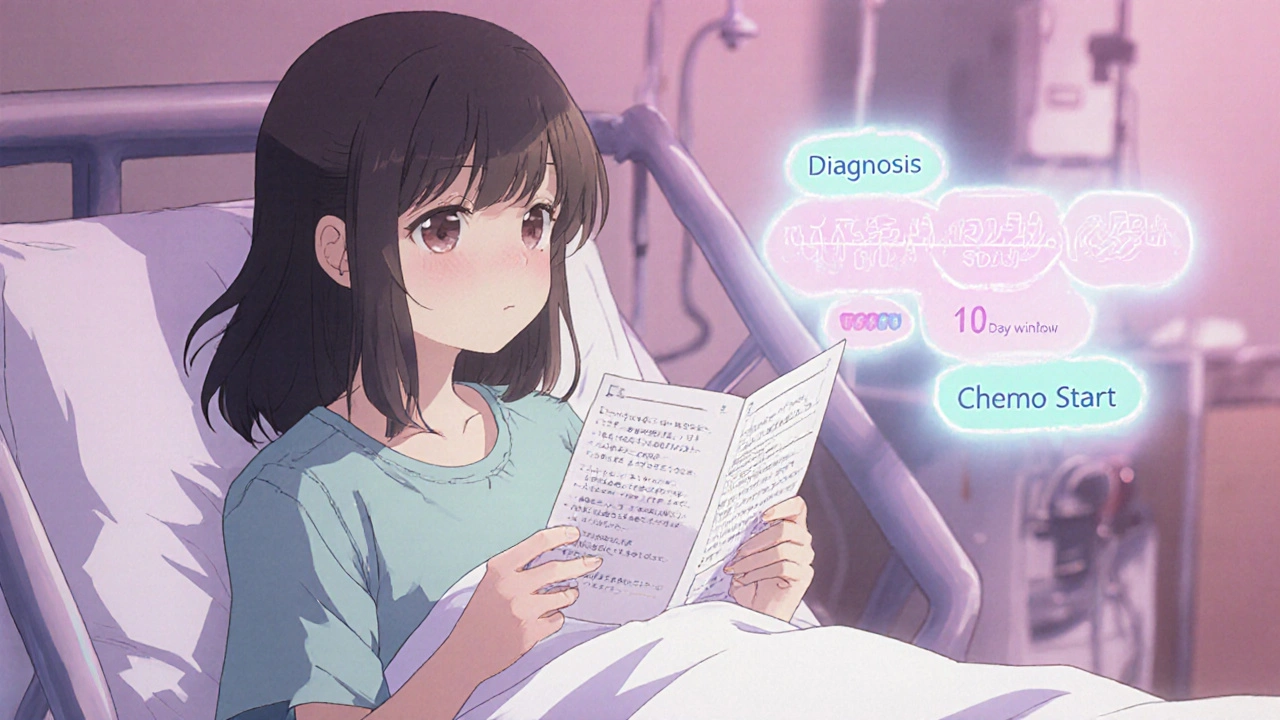
How Much Time Do You Really Have?
Most people assume they have weeks to decide. They don’t. In aggressive cancers like leukemia, doctors may need to start chemotherapy within 48-72 hours. That’s why referral to a fertility specialist should happen the same day as diagnosis. The average time to complete egg or embryo freezing is 10-14 days. But newer "random-start" protocols allow stimulation to begin at any point in the menstrual cycle, cutting the delay to about 11 days on average. For sperm banking, collection can be done in under 72 hours. If you wait more than 21 days after diagnosis, you’re at high risk of missing the window entirely. Data from MD Anderson Cancer Center shows 68% of young women regret not acting sooner.
What About Cost and Insurance?
Costs vary widely. Egg freezing can run $8,000-$15,000 per cycle, plus $500-$1,000 a year for storage. Sperm banking is cheaper-usually under $1,000. But here’s the reality: insurance doesn’t always cover it. In 24 U.S. states, laws require insurers to cover fertility preservation for cancer patients. But in the rest, you’re on your own. Medicaid covers it in only 12 states. Many patients report denials, even when their oncologist recommends it. Some clinics offer payment plans or discounts for cancer patients. Don’t assume it’s too expensive until you ask. And remember: freezing now might save you from paying for donor eggs or surrogacy later.
What’s New in Fertility Preservation?
Technology is moving fast. In 2023, the FDA approved the first closed-system vitrification device that cuts contamination risk by 92%. That’s a big deal-fewer infections mean safer storage. Researchers are also testing "in vitro activation" of frozen ovarian tissue, which could let you grow eggs in a lab instead of re-implanting tissue. This could be huge for women with BRCA mutations who want to avoid returning cancer-prone tissue to their bodies. Another promising area: artificial ovaries. A $4.7 million NIH trial is testing lab-grown ovarian structures in primates, with 68% follicle survival so far. These aren’t ready for humans yet, but they’re the next frontier.
Emotional and Practical Realities
It’s not just medical-it’s emotional. One Reddit user wrote: "I was diagnosed with breast cancer at 29. I had to choose between saving my life and saving my chance to be a mom. I didn’t freeze my eggs. Now I cry every time I see a baby." A 2022 study of 127 patients found that the stress of making these decisions on top of cancer treatment was overwhelming. Many felt rushed, uninformed, or alone. Support groups, counselors, and patient advocates can help. Don’t go through this alone. Ask your oncology team for a referral to a fertility counselor. They’re trained to help you weigh options without pressure.
What If You’re Under 18?
For children and teens, options are limited. Egg or sperm freezing isn’t possible before puberty. Ovarian tissue cryopreservation is the only proven option for girls. For boys, testicular tissue freezing is still experimental-no live births yet. But many hospitals now offer it as part of research programs. If your child is diagnosed with cancer, ask immediately: "Can we freeze ovarian or testicular tissue?" Even if it’s not guaranteed to work, it’s the only shot they’ll ever have.
What’s the Bottom Line?
If you’re facing chemotherapy and you want to have biological children someday, act fast. Talk to your oncologist on day one. Ask for a referral to a fertility specialist. Don’t wait for them to bring it up-many doctors still don’t. Know your options. Know your timeline. Know your rights. Even if you don’t use your frozen eggs or sperm now, having them stored gives you peace of mind. And for some, it gives them a future they thought they’d lost.
Can I still have kids after chemotherapy if I don’t freeze anything?
It’s possible, but not likely. About 30-80% of premenopausal women who receive alkylating agents (common in breast and lymphoma treatments) will go into early menopause. Men may have low or zero sperm counts after treatment. Some people regain fertility naturally, but it’s unpredictable. Freezing eggs, sperm, or tissue before treatment gives you control over your future fertility.
Does ovarian suppression (GnRHa) really work?
It helps, but it’s not a guarantee. Studies show it reduces the risk of early menopause by 15-20%. That means if 50% of women would normally lose their fertility, suppression might lower that to 30-35%. It’s best used alongside other methods like egg freezing, not instead of them. It also has side effects-hot flashes, mood swings, bone loss-that some find hard to tolerate.
How long can frozen eggs or embryos last?
There’s no expiration date. Frozen eggs and embryos have been successfully used after 10-20 years in storage. The freezing process (vitrification) stops biological aging. As long as they’re stored properly, they remain viable. Success depends more on the age of the woman when they were frozen than how long they’ve been frozen.
Is fertility preservation covered by insurance?
It depends on where you live and your insurance plan. In 24 U.S. states, laws require insurers to cover fertility preservation for cancer patients. In others, coverage is rare. Medicaid covers it in only 12 states. Always check with your insurer and ask your clinic for a pre-authorization letter. Many clinics offer financial aid or payment plans for cancer patients.
Can I do fertility preservation if I have hormone-sensitive cancer like breast cancer?
Yes. Special protocols exist to avoid raising estrogen levels too much during egg stimulation. Medications like letrozole can be used alongside fertility drugs to keep estrogen low. Many women with breast cancer have successfully frozen eggs or embryos and gone on to have healthy pregnancies. Talk to a specialist who has experience with cancer patients.
What if I’m not in a relationship? Can I still freeze my eggs?
Absolutely. Egg freezing doesn’t require a partner. You can use donor sperm later when you’re ready. Many single women choose this option to preserve their fertility without committing to a partner right now. It’s becoming one of the most common reasons for egg freezing among young cancer patients.

Gabriella Jayne Bosticco
November 18, 2025 AT 09:35Emanuel Jalba
November 18, 2025 AT 23:00Heidi R
November 20, 2025 AT 05:58Iska Ede
November 21, 2025 AT 11:01Denny Sucipto
November 21, 2025 AT 18:26Hal Nicholas
November 22, 2025 AT 21:27Louie Amour
November 23, 2025 AT 20:12Kristina Williams
November 23, 2025 AT 21:58Shilpi Tiwari
November 24, 2025 AT 16:35Christine Eslinger
November 25, 2025 AT 12:05Holly Powell
November 26, 2025 AT 17:49Brenda Kuter
November 28, 2025 AT 08:49Shaun Barratt
November 29, 2025 AT 06:08Sarah Frey
December 1, 2025 AT 05:55Kristi Joy
December 1, 2025 AT 19:21