Fish Oil and Omega-3s: What the Science Really Says About Heart Health
For years, fish oil supplements have been sold as a simple fix for heart health. Walk into any pharmacy and you’ll see shelves lined with bottles promising stronger hearts, lower cholesterol, and fewer heart attacks. But the truth is more complicated. The science hasn’t kept up with the marketing. Some studies say fish oil saves lives. Others say it does almost nothing. So what’s actually going on?
What Exactly Are Omega-3s?
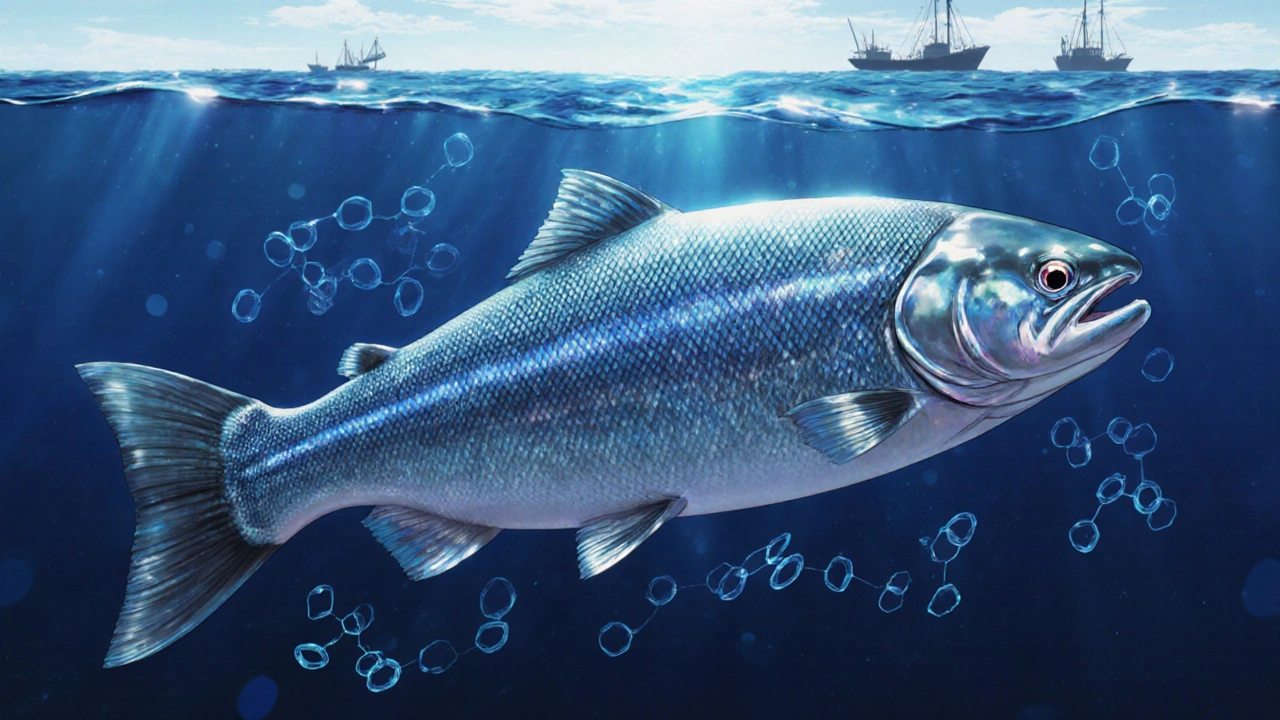
Omega-3 fatty acids are a type of fat your body can’t make on its own. That means you have to get them from food or supplements. The two most important kinds for your heart are EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid). These are found mostly in fatty fish like salmon, mackerel, sardines, and herring. There’s also ALA, a plant-based omega-3 in flaxseeds, chia seeds, and walnuts - but your body turns very little of it into EPA or DHA, so it doesn’t count as much for heart protection.
The American Heart Association has been talking about omega-3s for two decades. Their 2002 guidelines recommended about 1 gram of EPA and DHA daily for people with existing heart disease. That advice still stands - but only for certain groups. For everyone else, the story has changed.
The Big Studies That Changed Everything
In 2018, the REDUCE-IT trial shocked the medical world. It followed nearly 8,200 people with high triglycerides and existing heart disease or diabetes. They were given 4 grams a day of purified EPA (a drug called Vascepa). After five years, those taking EPA had 25% fewer heart attacks, strokes, and heart-related deaths compared to those taking a placebo. That’s a big deal. It led to FDA approval in December 2020 for this specific use.
But then came STRENGTH in 2020. This trial used 4 grams a day of a mix of EPA and DHA (Epanova). The results? No benefit at all. The trial was stopped early because it clearly wasn’t working. Why the difference? One theory: DHA might cancel out some of EPA’s benefits. No one’s tested pure DHA alone at high doses yet, so we don’t know if it’s helpful, harmful, or neutral.
Then there’s the 2023 Cochrane review - the most thorough analysis ever done. It looked at 79 studies with over 112,000 people. The conclusion? Long-chain omega-3s (EPA and DHA) have little to no effect on heart attacks, strokes, or death from heart disease. This wasn’t a small study. It was massive. And it found almost no benefit for the average person.
Who Actually Benefits?
If you’re a healthy adult with no heart problems, fish oil supplements probably won’t help you avoid a heart attack. The VITAL trial in 2018, which followed over 25,000 people, found no overall reduction in heart disease risk with 1 gram of omega-3s daily. But here’s the twist: among African American participants, heart attacks dropped by 77%. Why? Researchers think it might be linked to genetic differences in how the body processes omega-3s.
For people with high triglycerides (above 150 mg/dL), the story is different. The AHA recommends 2 to 4 grams of EPA and DHA daily - but only if you can’t get enough from diet alone. Prescription omega-3s like Vascepa or Lovaza are approved for this. Over-the-counter fish oil? You’d need 4 to 8 capsules a day to reach that dose. And most brands don’t even deliver that much.
People with heart failure may also benefit. A 2019 AHA advisory noted that omega-3s might reduce deaths from coronary heart disease and sudden cardiac arrest by about 10% when taken at 1 gram daily. That’s not a cure. But for someone already at high risk, it could matter.

Prescription vs. Over-the-Counter: The Real Difference
Not all fish oil is created equal. Prescription omega-3s like Vascepa are pure EPA. They’re tightly controlled, tested for purity, and dosed precisely. Over-the-counter supplements? They’re not regulated like drugs. A typical capsule has 300-500 mg of combined EPA and DHA. To get the 4 grams used in REDUCE-IT, you’d need 8-12 capsules a day. Most people won’t do that - and even if they do, the quality might be poor.
Consumer Reports tested 35 fish oil brands in early 2023. Twelve of them had oxidation levels higher than international safety limits. That means the oil was going bad - rancid fish oil doesn’t help your heart. It might hurt it. And while heavy metals like mercury are usually low in reputable brands, you can’t assume all supplements are safe.
Cost is another factor. Vascepa can run $300 a month, even with insurance. Over-the-counter fish oil? $10 to $50 a month. But if you’re not getting enough EPA to make a difference, you’re just spending money for nothing.
Side Effects and Risks
Fish oil isn’t harmless. Common complaints? Fishy burps, stomach upset, diarrhea. Around 27% of users report digestive issues. In clinical trials, 10-20% drop out because of side effects.
At high doses (over 3 grams daily), there’s a small but real risk of increased bleeding. That’s why people on blood thinners like warfarin should talk to their doctor before starting. And in 2022, a meta-analysis in JAMA Cardiology found a 0.4% absolute increase in atrial fibrillation - irregular heartbeat - among people taking high-dose omega-3s. That sounds small, but for someone already at risk for heart rhythm problems, it matters.
What Should You Do?
Here’s the practical breakdown:
- If you have heart disease or high triglycerides and your doctor says you need it - take Vascepa. It’s proven.
- If you’re healthy and want to prevent heart disease - skip the pills. Eat fish instead.
- If you’re African American and have no history of heart disease - talk to your doctor. The VITAL trial suggests you might benefit more than others.
- If you’re taking fish oil supplements now - check the label. Are you getting at least 1 gram of EPA and DHA? If not, you’re probably wasting your money.
For most people, the best source of omega-3s isn’t a bottle - it’s your plate. Two servings a week of fatty fish (like salmon, sardines, or trout) give you about 500 mg of EPA and DHA daily. That’s enough for general heart health. No pills needed.
Why the Confusion?
Why do some studies say fish oil works and others say it doesn’t? It comes down to three things:
- Dose matters. 1 gram won’t do the same thing as 4 grams.
- Form matters. Pure EPA works. EPA + DHA might not.
- Who you are matters. High-risk patients benefit. Healthy people don’t.
The supplement industry is worth over $5 billion. That’s a lot of money pushing the idea that fish oil is a miracle cure. But science doesn’t care about marketing. It cares about data. And right now, the data says: don’t take fish oil unless you have a clear medical reason.
The Bottom Line
Fish oil isn’t magic. It’s not useless. It’s context-dependent. For people with high triglycerides and heart disease, high-dose EPA can be life-saving. For everyone else, it’s probably just a waste of cash - and maybe even a little risky.
Don’t take fish oil because you saw an ad. Don’t skip it because you read a headline. Talk to your doctor. Get your triglycerides checked. Know your risk. Then decide - based on your body, not your wallet.
And if you’re not eating fatty fish at least twice a week - start. That’s the real heart-healthy habit. No bottle required.

Christopher Robinson
November 20, 2025 AT 13:59Love this breakdown. Seriously, most people don’t realize that fish oil supplements are basically the wellness equivalent of buying a ‘miracle’ weight-loss tea. 😅
My dad took 10 capsules a day for years - spent hundreds, got zero results. Then he started eating salmon twice a week and his triglycerides dropped like a rock. No pills. Just food.
Also, rancid fish oil? Yeah, that’s a thing. I learned the hard way when my fridge smelled like a seafood dumpster for a week. Never buying cheap brands again.
harenee hanapi
November 21, 2025 AT 02:30Oh please. Another ‘science says’ article that ignores the real truth - fish oil has saved countless lives in my family. My uncle had a heart attack at 48, took prescription omega-3s, and now he’s hiking in the Rockies at 65. You think some Cochrane review knows more than real-life survival stories? 😒
And don’t even get me started on how Big Pharma hates natural remedies. They don’t want you to know the truth - because they can’t patent fish.
Nick Lesieur
November 22, 2025 AT 09:44so like… if i’m healthy and take fish oil… i’m just a dumbass who got scammed by ads? 😅
also why does every article about this sound like a pharmaceutical ad? ‘Vascepa this. Epanova that.’ like i’m supposed to go to my doc and beg for a $300 prescription because my wallet’s crying.
Angela Gutschwager
November 23, 2025 AT 00:50Stop spending money on fish oil. Eat salmon. That’s it. 😘
Andy Feltus
November 24, 2025 AT 23:31It’s funny how we treat supplements like they’re moral choices - ‘good people take fish oil, bad people ignore science.’
The real question isn’t whether it works - it’s why we’re so desperate to outsource health to a pill. We’d rather swallow a capsule than change our diet, our stress levels, or our sleep. Fish oil becomes a proxy for self-care - a placebo for the guilt of not eating better.
And yet, we still buy it. Because it’s easier than facing the truth: your heart doesn’t need a bottle. It needs time. Quiet. Food that doesn’t come in a plastic pouch.
Dion Hetemi
November 25, 2025 AT 22:09Let’s be real - the only reason this debate even exists is because the supplement industry is a $5 billion Ponzi scheme built on half-baked science and celebrity endorsements.
REDUCE-IT showed EPA works. STRENGTH showed EPA+DHA doesn’t. Cochrane showed no benefit for average people. That’s not confusion - that’s a pattern. But the industry doesn’t care. They’ll keep selling 500mg capsules labeled ‘heart-healthy’ while laughing all the way to the bank.
And don’t even get me started on the ‘African American benefit’ being buried in a footnote. That’s not science - that’s systemic neglect. If this worked for white people, they’d be screaming it from rooftops. But since it’s a racial subgroup? ‘Hmm, interesting… move along.’
Meanwhile, people in food deserts can’t even afford salmon. So they buy fish oil. And the cycle continues. This isn’t about health. It’s about capitalism exploiting hope.
Timothy Reed
November 26, 2025 AT 18:39As someone who’s worked in cardiology for 18 years, I see this every day. Patients come in convinced fish oil is their magic bullet - then get shocked when their LDL hasn’t budged.
The truth is simple: if you’re at high risk - high triglycerides, history of heart attack, diabetes - then yes, high-dose prescription EPA is one of the most effective tools we have. But it’s not a substitute for statins, blood pressure control, or lifestyle changes.
And for the general public? The evidence is clear: no benefit. Save your money. Eat fish. Walk more. Sleep better. Those are the real interventions - not pills with vague labels and expired expiration dates.
Also, please check your supplement’s COA (Certificate of Analysis). Most don’t even list the actual EPA/DHA content. It’s the Wild West out there.
James Ó Nuanáin
November 27, 2025 AT 08:08How utterly predictable. Another American article dismissing the wisdom of centuries of dietary tradition in favor of clinical trials conducted by overpaid academics with industry ties.
In the UK, we’ve known for decades that omega-3s from wild-caught fish are essential - not just for the heart, but for cognitive function, mood, and even joint health. The Cochrane review? A product of American data-mining with insufficient sample diversity. And let’s not forget: the REDUCE-IT trial was funded by the manufacturer of Vascepa - yet somehow, the STRENGTH trial, which failed, is treated as gospel?
It’s no wonder the American healthcare system is so broken. You treat medicine like a spreadsheet, not a science rooted in human biology. Meanwhile, in Scandinavia, children are given fish oil from infancy. Their heart disease rates? A fraction of yours.
Perhaps it’s time America stopped outsourcing its health to Silicon Valley wellness influencers and listened to the old ways - the ones that didn’t require a prescription.
Kara Binning
November 28, 2025 AT 15:16Okay, but what about the fact that fish oil makes you burp? Like… is that the real cost of heart health? 😭
I tried it. For three months. Smelled like a seafood market after a hurricane. My dog started avoiding me. My partner asked if I was ‘on something.’ I gave up. Now I just eat tuna sandwiches. Same result. Zero burps. And I still have a pulse.
Also, why is everyone acting like this is new? My grandma took cod liver oil in the 1950s. She lived to 97. She didn’t know what EPA was. She just knew it was ‘good for you.’ Maybe we’re overthinking this.