Fungal Skin Infections: Candida, Ringworm, and Antifungals Explained
More than 1 in 5 people worldwide have a fungal skin infection right now. It’s not rare. It’s not weird. It’s not something you caught from being dirty. Fungal skin infections like Candida and ringworm are everywhere - in locker rooms, on pets, in warm skin folds, and even in healthy people with normal hygiene. The problem? Most of them get misdiagnosed. You think it’s eczema. Or a rash. Or heat irritation. But it’s fungus. And if you don’t treat it right, it comes back. Again. And again.
What’s Actually Growing on Your Skin?
Fungal skin infections fall into two main groups: dermatophytes (ringworm) and yeasts (Candida). They look different, act different, and need different treatments. Confusing them is the number one reason treatments fail.
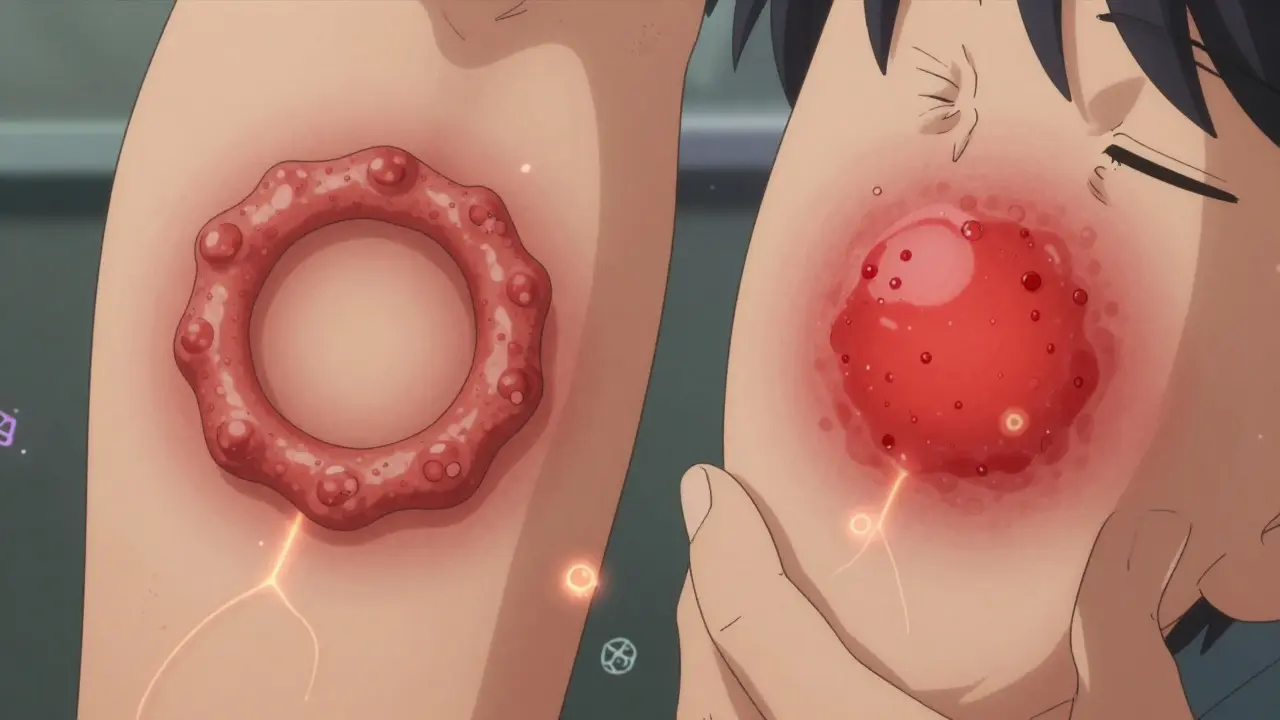
Ringworm - yes, that’s the name - isn’t caused by worms. It’s caused by fungi called dermatophytes. These fungi eat keratin, the protein in your skin, hair, and nails. That’s why they stick to those areas. The classic sign? A red, scaly ring with a raised edge and a clearer center. It’s circular. It itches. It spreads. You can get it on your scalp (tinea capitis), feet (athlete’s foot), groin (jock itch), or nails (onychomycosis). Trichophyton fungi cause 80-90% of cases. Cats and dogs are common carriers, especially in kids.
Candida infections, on the other hand, are yeast overgrowths. Candida albicans is the usual culprit. These fungi love warm, moist places: under your breasts, in your armpits, between your toes, and especially in diaper areas. The rash looks different - not a ring, but a bright red, wet, sometimes pimpled patch with tiny red spots around the edges (satellite pustules). It’s not usually scaly. It’s often painful. And it doesn’t respond to steroid creams, which many people try first.
Who Gets These Infections - And Why?
It’s not just about cleanliness. Risk factors matter more.
- Diabetes increases your chance of Candida infections by 2.5 times. High sugar levels feed the yeast.
- People with weak immune systems - from HIV, chemo, or steroids - are 3 to 5 times more likely to get severe or recurring infections.
- Wearing tight, sweaty clothes? That’s a recipe for jock itch or intertrigo (Candida in skin folds).
- Older adults (over 60) are far more likely to get athlete’s foot. Skin gets thinner, drier, and less protective.
- Infants under 1 year? Up to 25% get Candida diaper rash. It’s common, not a parenting failure.
And yes, you can catch ringworm from pets. About 20-30% of childhood cases come from cats or dogs. If your dog is scratching and losing patches of fur, it might not be allergies - it could be ringworm.
How Do Doctors Know It’s Fungus?
Many doctors guess. That’s the problem. A 2022 study found primary care doctors correctly identify ringworm only half the time. Dermatologists? 85-90% accurate.
The gold standard is the KOH test. A doctor scrapes a bit of skin, puts it on a slide with potassium hydroxide, and looks under a microscope. Fungal threads show up instantly. It’s fast, cheap, and works in 70-80% of cases.
For stubborn cases - especially nail infections - a fungal culture is needed. But it takes 2-4 weeks. That’s why people give up. Molecular tests are becoming more common now, giving results in days instead of weeks.
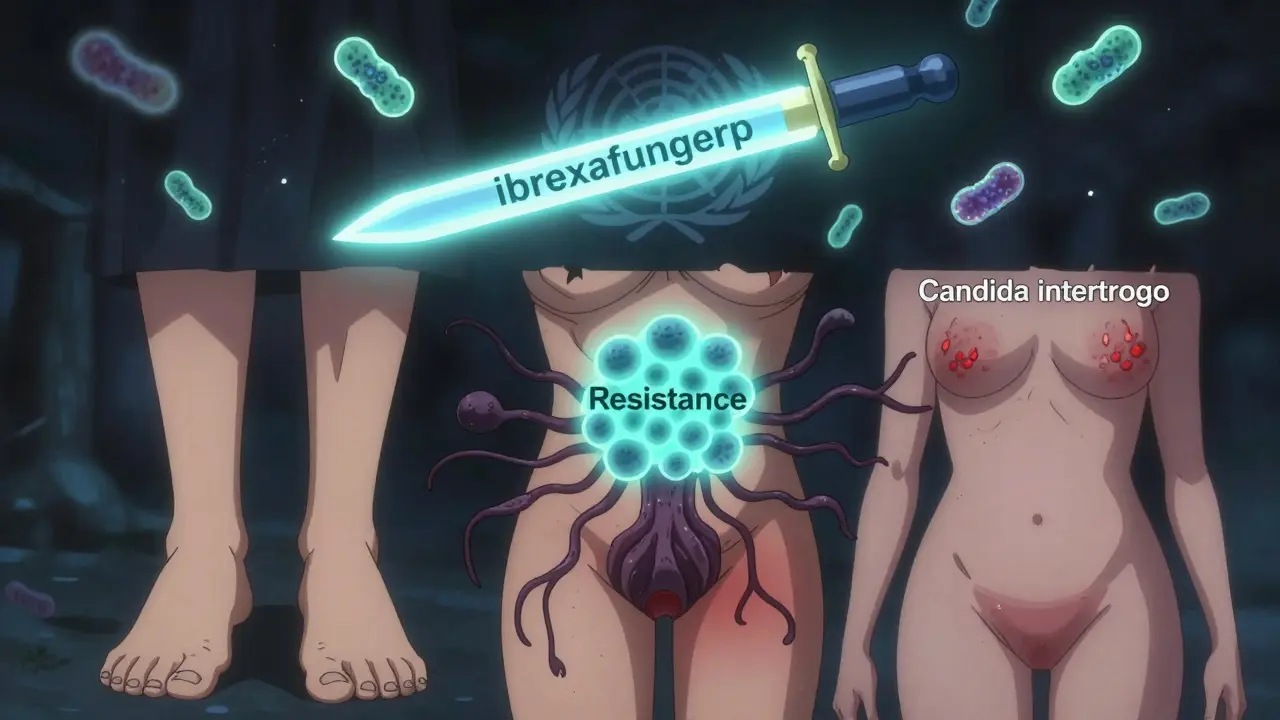
Here’s the catch: if your rash looks exactly like classic ringworm or Candida intertrigo, many dermatologists will just start treatment without testing. Why? Because waiting weeks for a culture means the infection spreads. If it’s not fungus, the antifungal won’t hurt - it just won’t work. And you’ll know quickly.

Antifungals: What Works, What Doesn’t
Not all antifungals are the same. You can’t use the same cream for athlete’s foot and a yeast rash.
For ringworm (dermatophytes):
- Topical: Terbinafine (Lamisil) or clotrimazole (Lotrimin). Apply twice daily for 1-2 weeks (body) or 4-6 weeks (feet). Cure rates: 70-90%.
- Oral: Terbinafine (250 mg daily) for 2-6 weeks. Required for nail infections or widespread cases. Liver checks are needed - about 1-2% of people get mild liver enzyme changes.
For Candida:
- Topical: Clotrimazole, miconazole, or nystatin cream. Apply twice daily for 1-2 weeks. Works well for skin folds and diaper rash.
- Oral: Fluconazole (one pill, sometimes repeated). Used for persistent or mucosal infections (like vaginal yeast). But resistance is rising.
Here’s a reality check: most people stop using antifungals too early. A 2022 JAMA Dermatology study found only 45% of patients finished their full course. You feel better in a few days. So you stop. The fungus is still there. It comes back. And now it’s tougher to kill.
What’s New in Treatment?
Things are changing fast.
In April 2023, the FDA approved ibrexafungerp (Brexafemme) for recurrent vaginal yeast infections. It’s the first new oral antifungal in over 20 years. In trials, it cut recurrence by half over 48 weeks.
For tinea versicolor (a different yeast rash), ciclopirox is now preferred over selenium sulfide shampoos. It’s more effective and less messy.
And then there’s the scary part: Candida auris. This multidrug-resistant yeast is spreading in hospitals. It colonizes skin, survives on surfaces for weeks, and doesn’t respond to common antifungals. It’s been detected in 27 U.S. states. It’s not common in healthy people - but if you’re in a hospital or nursing home, it’s a real threat.
Resistance is growing. About 5-7% of Trichophyton rubrum (the most common ringworm fungus) in North America is now less sensitive to terbinafine. Doctors are watching closely.
What Patients Are Saying
Real people share what works - and what doesn’t.
On Reddit, 68% of users with ringworm cleared it in 2-3 weeks with over-the-counter terbinafine. But 22% needed a prescription pill. Common complaints? Recurrence (35%) and the long treatment time for nail infections (31% said it was too long).
For Candida diaper rash and skin folds, 78% of users in a survey said clotrimazole worked well. But many reported being misdiagnosed first - as eczema, psoriasis, or heat rash. That’s why they wasted weeks on steroid creams that made it worse.
And here’s an unexpected trend: people with recurring vaginal yeast infections are turning to probiotics. A June 2023 Instagram poll of 850 people showed 65% had fewer outbreaks when they added Lactobacillus supplements to their antifungal treatment. Science is still catching up, but the pattern is strong.
What to Do If You Think You Have One
Here’s a simple guide:
- Look at the rash. Is it a red ring with a raised edge? Likely ringworm. Is it a wet, red patch with tiny red bumps around it? Likely Candida.
- Don’t use steroid creams (like hydrocortisone). They make fungal infections worse.
- Start with an OTC antifungal: terbinafine for ringworm, clotrimazole for yeast.
- Apply it daily, even after it looks better. Full course = full cure.
- If it doesn’t improve in 2 weeks, or if it keeps coming back, see a doctor. Get a KOH test.
- Keep skin dry. Change socks. Dry between toes. Wear loose cotton underwear. Fungus thrives in dampness.
And if you have diabetes or a weak immune system? Don’t wait. Get checked early. These infections can become serious fast.
The Bigger Picture
Fungal skin infections aren’t glamorous. But they’re everywhere. The global antifungal market hit $14.7 billion in 2022. Over-the-counter sales in the U.S. alone were $1.8 billion. People are spending money because they’re frustrated. They’ve been misdiagnosed. They’ve tried the wrong thing.
But awareness is rising. Research is getting more funding. The WHO now lists fungal pathogens as a global health priority. New drugs are in development. And the more we understand - that these aren’t just "dirty skin" problems, but biological infections with real patterns - the better we can treat them.
You don’t need to live with a rash that won’t go away. It’s not your fault. It’s not contagious because you’re unclean. It’s a fungus. And with the right treatment, it can be gone - for good.
Can fungal skin infections go away on their own?
Rarely. While some mild cases might improve slightly over time, fungal infections rarely clear completely without treatment. The fungi are persistent and will keep growing as long as conditions are warm and moist. Left untreated, they often spread to other areas or become chronic, leading to recurring rashes and increased risk of secondary bacterial infections.
Is ringworm contagious?
Yes. Ringworm spreads easily through direct skin contact with an infected person or animal, or by touching contaminated surfaces like towels, gym mats, or shower floors. Pets, especially cats, are common carriers. It’s not as contagious as the flu, but it doesn’t take much - a shared comb, a towel left on the floor, or a handshake with someone who has athlete’s foot can pass it along.
Can I use athlete’s foot cream for jock itch?
Yes, you can. Both are caused by the same type of fungi (dermatophytes), and the same antifungal creams - like terbinafine or clotrimazole - work for both. The key is to apply it consistently and keep the area dry. Jock itch is just ringworm in the groin, so the treatment is identical.
Why does my rash keep coming back after treatment?
Most often, it’s because treatment stopped too soon. Fungi can survive under the skin surface even after the visible rash fades. You need to use the cream for the full recommended time - even if it looks gone. Other reasons: not drying skin properly, wearing tight synthetic clothes, or re-exposure (like walking barefoot in a shared shower). For Candida, uncontrolled diabetes or antibiotics can also trigger recurrence.
Are natural remedies like tea tree oil effective?
Some studies show tea tree oil has antifungal properties in the lab, but there’s no strong evidence it works reliably in real-world skin infections. It can irritate sensitive skin. For a confirmed fungal infection, stick with proven antifungals like clotrimazole or terbinafine. Natural remedies shouldn’t replace medical treatment - they’re not regulated, and their potency varies wildly.
How long does it take to cure a fungal nail infection?
Nail infections take months - not weeks. Oral terbinafine typically requires 6-12 weeks for toenails and 3-6 weeks for fingernails. But the nail has to grow out completely before you see the full result. That can take 6-12 months. Patience is key. Topical treatments alone rarely work for nails. You need oral medication for a real cure.
Can I prevent fungal skin infections?
Yes. Keep skin dry, especially between toes and in skin folds. Wear moisture-wicking socks and change them daily. Avoid walking barefoot in public showers or locker rooms. Don’t share towels, shoes, or hairbrushes. If you have diabetes, manage your blood sugar - it’s one of the biggest preventable risk factors. Regularly check pets for bald patches - they can be silent carriers.

Dave Alponvyr
December 16, 2025 AT 10:51Used hydrocortisone on my jock itch for a month. Turned into a circus tent. Then tried Lamisil for 3 days and called it quits. Fungus won. Lesson learned: don't be lazy with antifungals.
Arun ana
December 17, 2025 AT 05:20My cousin got ringworm from our cat. We thought it was just dry skin. Took 3 months to figure it out. Now we check the dog every week. 🐶🩹
Kim Hines
December 19, 2025 AT 01:48I had that Candida rash under my breast for 6 months. Doctor said it was eczema. I cried in the parking lot. Started clotrimazole on my own. Gone in 10 days.
Cassandra Collins
December 19, 2025 AT 11:14Did you know the FDA approved ibrexafungerp because Big Pharma wants you to keep buying antifungals forever? They're hiding the real cure - alkaline diets and magnetic therapy. I've been yeast-free for 2 years since I stopped eating sugar and wore copper socks. They don't want you to know this.
Joanna Ebizie
December 20, 2025 AT 12:29People who don't finish their antifungal course are just lazy. You think your skin is too sensitive for a cream? No, you're just too lazy to care. Stop making excuses and treat it right.
Souhardya Paul
December 22, 2025 AT 03:56Biggest thing I learned? Ringworm and jock itch are the same bug. I used athlete’s foot cream on my groin and it worked fine. No need to overcomplicate it. Just keep it dry and don’t stop the cream early. Also, if your dog’s got bald spots, get it checked. My nephew got ringworm from our golden retriever. We thought it was just allergies. Took weeks to figure out. Now we wipe his paws after walks. Simple.
And Candida? Don’t even think about steroid cream. I tried it. Made it worse. Like pouring gasoline on a fire. Clotrimazole is cheap, works great, and doesn’t make your skin melt. Just use it like the label says. Even if it looks gone. Two weeks minimum.
Also, if you’re diabetic? This is your #1 skin issue. Blood sugar control is the real antifungal. No cream will fix it if you’re eating donuts every day. I’ve seen too many people get the same rash 3 times a year because they won’t touch their diet.
And yes, nail infections suck. They take forever. But if you skip the oral meds and just use cream? You’re wasting time. Oral terbinafine isn’t perfect, but it’s the only thing that actually kills the fungus under the nail. Liver check? Yeah, get one. But most people are fine. Don’t let fear stop you from getting better.
Probiotics for yeast? I started taking them after my third vaginal infection. Haven’t had one in 14 months. Not magic. But it helped. Science is catching up. Stop acting like natural stuff is always fake. Sometimes it just takes time to prove it.
And if you’re in a hospital? Watch out for Candida auris. It’s scary. But it’s not in your living room. Don’t panic. Just wash your hands. Seriously. Hand sanitizer works. It’s not conspiracy. It’s biology.
Bottom line: Fungus isn’t your fault. It’s not dirty. It’s just there. And it’s stubborn. But it’s beatable. You just have to be consistent. No shortcuts. No magic. Just patience and the right cream.
Hadi Santoso
December 23, 2025 AT 19:10My grandma in Indonesia used turmeric paste on her fungal rash. Said it worked. I tried it once. Made my skin yellow for a week. Didn’t kill the fungus. But hey, at least I looked like a Halloween pumpkin. Maybe it’s the cultural thing. In the US we go for pills and creams. In Bali they go for spices and prayers. Both have their place, I guess.
But honestly? The KOH test is the real MVP. My dermatologist did it in 2 minutes. No waiting. No guesswork. Just a quick scrape and boom - there’s the fungus. Why don’t more docs do this? Probably because it’s too easy and doesn’t make them look smart.
And yeah, pets. I had a cat that shed like crazy. Never thought it was ringworm. Turns out, she had a patch behind her ear. Took me 3 months to notice. Now I check my dog every time he shakes. Just a quick glance. Saves so much hassle.
Also - socks. Cotton socks. Every day. No synthetic crap. I swear, switching to cotton socks cut my athlete’s foot flare-ups by 80%. It’s not sexy advice. But it works.
And if you’re on steroids? Watch out. I was on prednisone for asthma and got a full-body Candida rash. Felt like I was melting. Doctor didn’t connect it. Took me reading this post to realize. Don’t be like me. Ask about fungus if you’re immunosuppressed.
Dylan Smith
December 25, 2025 AT 02:24Why is it always the same people who get these infections? It’s not random. It’s lifestyle. You wear tight pants all day. You don’t dry off after showering. You eat sugar like candy. You don’t change your underwear. Stop blaming the fungus. You’re the problem. Fix your habits before you buy another tube of cream.
And stop using tea tree oil. It’s not a miracle. It’s a scam. People think natural means better. It doesn’t. It means unregulated. I’ve seen people burn their skin trying to cure ringworm with essential oils. You want to treat a fungus? Use a drug. Not a perfume.
Also - if you’re using steroid cream for a rash and it gets worse? That’s not a coincidence. That’s biology. You’re feeding the fungus. Stop it. Now. I’m not being mean. I’m being real. You’re wasting time and making it worse.
And yes, nail infections take months. So what? You wait 3 months for a new phone. You wait 6 months for a tattoo. But you won’t wait 3 months for healthy nails? You’re choosing comfort over function. Grow up.
And if you think probiotics are a cure? They’re a helper. Not a replacement. You still need antifungals. Stop looking for shortcuts. Fungus doesn’t care about your Instagram detox trend.
Mike Smith
December 25, 2025 AT 16:37As a healthcare professional, I cannot emphasize enough the importance of completing the full course of antifungal therapy. The clinical data is unequivocal: premature discontinuation is the leading cause of treatment failure and recurrence. Patients who adhere to the prescribed regimen achieve cure rates exceeding 90%. Those who do not - regardless of symptom resolution - risk developing resistant strains and chronic infection. This is not a suggestion. It is a medical imperative.
Furthermore, the integration of diagnostic tools such as the KOH preparation into primary care workflows is not only cost-effective but also clinically superior to empirical treatment. Delayed diagnosis leads to increased transmission, prolonged suffering, and higher overall healthcare expenditures. We must prioritize education and accessibility.
For patients with comorbidities such as diabetes or immunosuppression, proactive screening and early intervention are not optional - they are life-preserving. Fungal infections in these populations can escalate rapidly, leading to systemic involvement. Vigilance is not paranoia. It is professionalism.
Lastly, while emerging therapies such as ibrexafungerp represent significant advances, they do not replace foundational principles: hygiene, adherence, and accurate diagnosis. Innovation must be paired with discipline. Let us not mistake novelty for necessity.
Elizabeth Bauman
December 25, 2025 AT 20:28Did you know that the WHO labeled fungi as a global health threat because of a secret agenda to push expensive drugs? They don’t want you to know that sunlight and sea salt cure everything. I’ve been using ocean water on my rash since 2021. No more fungus. No more pills. The government doesn’t want you to know this because Big Pharma owns the FDA. Check the patents. Look at the funding. It’s all connected. And they’re coming for your skin next.
Dave Alponvyr
December 25, 2025 AT 23:49LOL at the sea salt cure. I tried that. My skin burned for a week. Fungus didn’t care. Still got the cream.