How Lower Generic Drug Prices Improve Patient Adherence and Cut Healthcare Costs

When a patient skips a dose because the pill costs too much, it’s not just a personal choice-it’s a system failure. Every year, generic drug prices save billions in healthcare spending, but their real power lies in something quieter, deeper: they get people to take their medicine. And when people take their medicine as prescribed, hospitals see fewer emergencies, doctors see fewer complications, and lives get saved.
Why Cost Stops People From Taking Their Medicine
It’s simple math: if your copay for a heart medication jumps from $5 to $75, you’re more likely to skip doses, delay refills, or skip the prescription altogether. A 2023 JAMA Network Open survey of over 2,100 adults found that nearly one in three (32.7%) admitted to cutting back on meds because of cost. That’s not laziness. That’s survival. People choose between food, rent, and pills-and too often, pills lose. The data doesn’t lie. For every $10 increase in out-of-pocket cost, adherence drops by 2% to 4%. For drugs like GLP-1 agonists used in diabetes, each $10 rise cuts adherence likelihood by 3.7% and pushes emergency room visits up by 5.2%. These aren’t abstract numbers. They’re real people showing up at hospitals because their blood sugar spiraled out of control-because they couldn’t afford the daily pill that could’ve kept them stable.Generics Aren’t Cheaper Because They’re Weaker-They’re Cheaper Because They’re Smart
Generic drugs aren’t knockoffs. They’re exact copies. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent-within 80% to 125% of the brand drug’s performance. In other words, if your doctor prescribes Lipitor, and you take generic atorvastatin, your body can’t tell the difference. And yet, generics cost 80% to 85% less. That’s not a discount. That’s a revolution. In the U.S., generics make up 90% of all prescriptions filled-but only 23% of total drug spending. From 2009 to 2019, they saved the system $643 billion. That’s money that didn’t go to ERs, hospital stays, or dialysis machines. That’s money that stayed in people’s pockets.Real Stories: From $75 to $5-And Back to Life
One Reddit user, u/HeartHealthJourney, shared how switching from brand-name Crestor ($75 copay) to generic rosuvastatin ($5 copay) changed everything. Before the switch, they were missing 3 to 4 doses a week. After? Perfect adherence for 11 months straight. No more guilt. No more panic before payday. Just a steady, affordable way to manage their cholesterol. That’s not an outlier. A 2011 study by Hershman et al. looked at women taking aromatase inhibitors for early-stage breast cancer. Those on brand-name drugs had a 22.3% discontinuation rate. Those on generics? Just 17.8%. Adherence rates jumped from 68.4% to 73.1%. That’s not a small difference. That’s the difference between survival and relapse.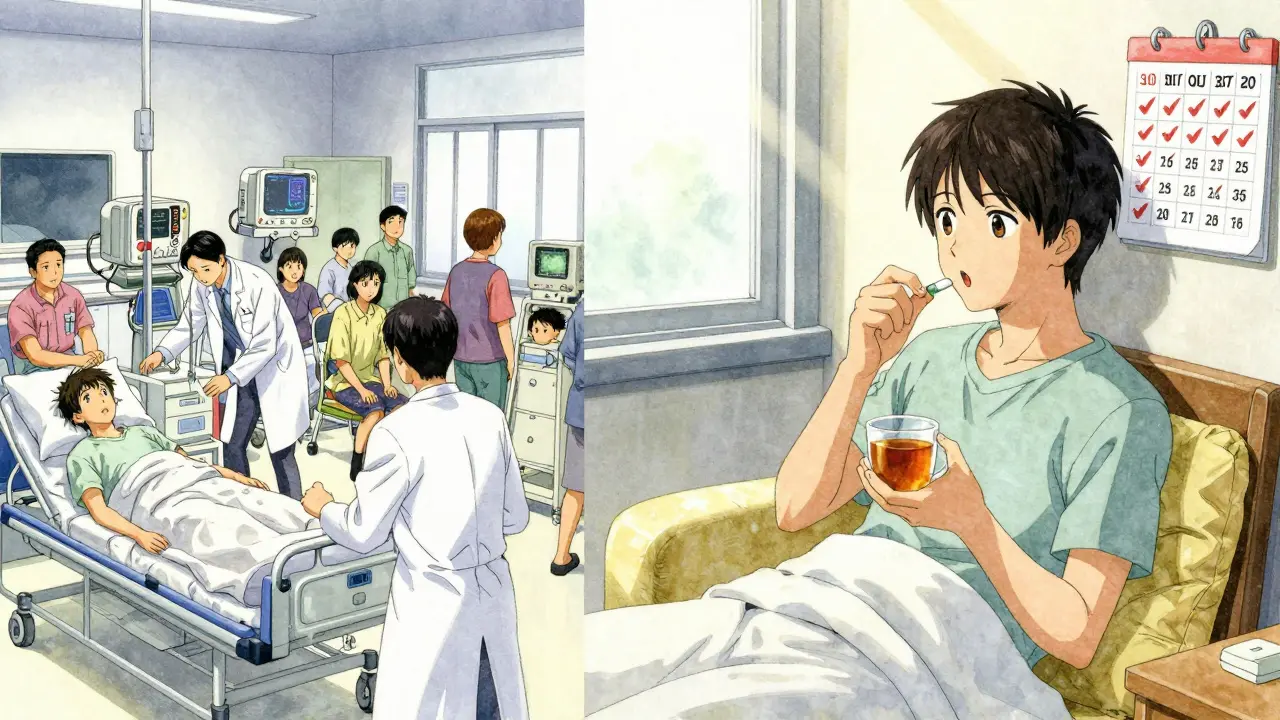
How Insurance Tiers Make or Break Adherence
Insurance plans don’t treat all drugs the same. They use “tiers.” Tier 1? Usually generics. $5 to $10 copay. Tier 2 or 3? Brand-name drugs. $40 to $100. Tier 4? Specialty drugs. $200+, sometimes more. When a drug moves from Tier 2 to Tier 1, adherence shoots up. In a landmark 2012 study by Chen et al., Medicare beneficiaries on statins saw a 5.9% increase in adherence-measured by proportion of days covered-after their brand-name statins were moved to the lowest-cost tier. That’s not a fluke. That’s a pattern repeated across heart disease, diabetes, depression, and high blood pressure. The reason? Cost isn’t just a number. It’s a barrier. When the price drops, the barrier disappears. People refill. They take it daily. They feel better. And the system saves money because fewer people end up in the hospital.What Happens When People Don’t Take Their Meds
Non-adherence isn’t just inconvenient. It’s deadly. Up to 50% of treatment failures are due to patients not taking their meds as prescribed. In the U.S., that contributes to more than 100,000 preventable deaths every year-and costs between $100 billion and $300 billion in avoidable healthcare spending. Think about it: a person with high blood pressure skips doses because they can’t afford the $80 copay. Their pressure stays high. A year later, they have a stroke. The hospital bill? $50,000. The rehab? Another $20,000. The lost income? Unquantifiable. Meanwhile, the monthly pill cost? $5. That’s the math no one talks about.How Systems Are Fixing This-And Where They’re Still Falling Short
Some changes are working. The Inflation Reduction Act of 2022 capped insulin at $35 a month. Starting in 2025, Medicare Part D will cap out-of-pocket drug spending at $2,000 a year. These policies alone could improve adherence for over 1.4 million seniors. Real-time benefit tools (RTBTs) are another breakthrough. These are apps or systems doctors use during appointments to see exactly what a patient’s copay will be for a drug-before they write the prescription. Pilots show a 12% to 15% boost in adherence when prescribers can choose lower-cost options on the spot. But problems remain. Many patients still don’t trust generics. They think cheaper means weaker. The FDA’s “It’s Okay to Use Generics” campaign helps, but it’s not enough. Insurance formularies are still confusing. A drug might be generic, but if it’s not on your plan’s preferred list, you pay more. Tools like GoodRx help patients compare prices across pharmacies-but not everyone knows to use them.The Bigger Picture: Generics Are the Foundation of Affordable Care
Americans pay 256% more for brand-name drugs than people in other rich countries like Canada, Germany, or the UK. Meanwhile, generic prices in the U.S. have stayed stable, even as brand-name drugs skyrocketed. From 2022 to 2023, over 4,200 drug prices rose-nearly half outpaced inflation by a wide margin. But generics? They kept their promise: safe, effective, and cheap. The future is clear: if we want better health outcomes and lower costs, we need to make generics the default-not the backup. That means training doctors to prescribe them first. It means simplifying insurance tiers. It means educating patients that generics aren’t second-rate-they’re second-to-none.What You Can Do-Even If You’re Not a Doctor or Policymaker
If you or someone you know is struggling to afford medication:- Ask your pharmacist: “Is there a generic version?”
- Use GoodRx or SingleCare to compare prices at nearby pharmacies-sometimes the cash price is lower than your copay.
- Ask your doctor: “Can we switch to a lower-cost option?”
- If you’re on Medicare, check if your drug is covered under the new $2,000 out-of-pocket cap starting in 2025.
- Don’t be ashamed to talk about cost. Over half of people who skip meds because of price say they’d feel “moderately or extremely upset” if their doctor didn’t ask about affordability.
It’s Not About Saving Money-It’s About Saving Lives
Lower generic prices aren’t just good economics. They’re good medicine. When people can afford their pills, they live longer, healthier lives. The system saves money. Hospitals get less crowded. Families sleep better at night. The data is overwhelming. The stories are real. And the solution? It’s already here. Generics work. They’re safe. They’re cheap. And they’re the most powerful tool we have to fix a broken system-one pill at a time.Do generic drugs work as well as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent-within 80% to 125% of the brand drug’s performance. Millions of people use generics every day with the same results as brand-name drugs.
Why do some people still prefer brand-name drugs?
Some people believe brand-name drugs are stronger or more reliable, even though there’s no scientific evidence to support that. Others have had a bad experience with a generic from a different manufacturer and assume all generics are the same. But generics are held to the same strict standards. If one generic doesn’t work well for you, trying another brand of the same generic might help.
How much can I save by switching to a generic?
On average, you’ll save 80% to 85%. For example, if a brand-name statin costs $150 a month with a $75 copay, the generic might cost $25 with a $5 copay. That’s $70 saved every month-or $840 a year. For chronic conditions, those savings add up fast.
Can I ask my doctor to prescribe a generic instead?
Absolutely. You have the right to ask. Many doctors already do this as standard practice, especially for conditions like high blood pressure, cholesterol, diabetes, and depression. If your doctor doesn’t mention generics, bring it up. Say: “Is there a lower-cost generic option that works just as well?”
What if my insurance won’t cover the generic?
Sometimes insurance plans have restrictions, like requiring you to try a brand-name drug first. If that’s the case, ask your doctor to file a prior authorization or appeal. You can also check if the manufacturer offers a patient assistance program. Or use tools like GoodRx to find the lowest cash price-even if your insurance doesn’t cover it.
Are there cases where generics don’t work as well?
Rarely. For most medications, generics are just as effective. In a few cases-like certain seizure or thyroid medications-small differences in inactive ingredients might affect how the drug is absorbed. But even then, switching between generics from different manufacturers can cause issues. If you notice a change in how you feel after switching, tell your doctor. Don’t assume it’s your fault. It’s a medical issue, not a personal failure.
How do real-time benefit tools help with adherence?
Real-time benefit tools show your doctor exactly what your copay will be for a drug before they write the prescription. That means they can choose a lower-cost option right then and there-instead of you finding out at the pharmacy and deciding not to fill it. Studies show this cuts missed prescriptions by 12% to 15% and improves adherence significantly.
Why don’t more doctors use these tools?
Many don’t have access, or their electronic health record system doesn’t integrate with them. Others aren’t trained to use them or don’t have time during appointments. But as more systems adopt these tools and Medicare expands coverage, adoption is growing. Patients who ask for cost transparency are helping push this change forward.

wendy parrales fong
December 27, 2025 AT 05:09It’s wild how something so simple-like switching to a generic-can change your whole life. I’ve seen friends choose between rent and pills. No one should have to make that call.
Generics aren’t ‘cheap meds.’ They’re smart meds. And we need to stop acting like they’re second-class.
My grandma takes her blood pressure generic every day. No drama. No panic. Just life.
Why are we still treating affordability like a bonus feature and not a baseline?
Jeanette Jeffrey
December 28, 2025 AT 18:07Oh please. You think generics are some magical solution? I’ve had one that made me dizzy for a week. The brand name? Perfect. Turns out ‘same active ingredient’ doesn’t mean ‘same experience.’
Also, why are we pretending people don’t have placebo effects? If you believe the brand works better, it probably does. Psychology matters more than FDA paperwork.
Stop romanticizing cost-cutting like it’s a virtue. Sometimes you pay for peace of mind.
Shreyash Gupta
December 30, 2025 AT 16:28Bro… I’m from India. We’ve been using generics since the 90s. 💯
My uncle took generic metformin for 15 years. No issues. No drama. Just lived.
But y’all act like generics are some newfangled hack? 😂
Meanwhile, your insulin costs $300 and you’re shocked? LMAO.
Stop acting like the US is the first country to figure out affordability.
Also, GoodRx? We had that in 2003. Called ‘local pharmacy.’
Ellie Stretshberry
December 31, 2025 AT 01:33i just want to say thank you for writing this
i’ve been skipping my antidepressants because of the copay and i didn’t know i could ask for a generic
my doctor never brought it up and i was too ashamed to say anything
but now i’m gonna go ask tomorrow
you’re right it’s not about saving money it’s about surviving
thank you
Zina Constantin
December 31, 2025 AT 21:23This is the kind of public health insight we need more of. Not just data-real human impact.
Generics are the unsung heroes of modern medicine. They’re the reason millions of Americans aren’t bankrupt or dead.
And yet, we treat them like discount aisle junk.
Imagine if we celebrated generics like we celebrate electric cars or vaccines. ‘Hey, your pill saved your life? Nice. Here’s a medal.’
We need a cultural shift. Not just policy. We need to stop stigmatizing affordability.
It’s not ‘cheap.’ It’s brilliant.
Dan Alatepe
January 1, 2026 AT 10:55OMG I just had a breakdown at the pharmacy yesterday 😭
My cholesterol med went from $5 to $78. I cried. Right there. In front of the guy selling cough drops.
Then I found the generic. $4.50. Same pill. Same results.
Why does the system make us suffer before we get the truth?
Someone needs to write a movie about this.
And no, I’m not ‘weak’ for crying. I’m just tired of being punished for being poor.
Angela Spagnolo
January 2, 2026 AT 12:34...I just want to say... that the part about insurance tiers... it really hit me...
...I didn’t realize... that moving a drug to tier one... could increase adherence by almost 6%...
...and that’s... that’s like... hundreds of thousands of people...
...who didn’t have strokes...
...because someone... finally... made the right decision...
...I’m just... so... grateful...
...thank you... for writing this...
...I’m going to tell my sister...
...she’s on a statin...
...and she’s scared to switch...
...but now... I think she’ll listen...
Michael Bond
January 3, 2026 AT 17:55Generics work. End of story.
Kuldipsinh Rathod
January 5, 2026 AT 12:16Man, I’m from Delhi and we’ve been using generics for decades. My dad’s on one for diabetes since 2008. No issues.
But here in the US, people treat generics like they’re haunted. It’s wild.
And don’t get me started on how pharmacies charge $100 for a 30-day supply when the generic costs $3 wholesale.
It’s not the drug. It’s the system.
SHAKTI BHARDWAJ
January 6, 2026 AT 20:55YOU’RE ALL WRONG AND I’M SICK OF THIS NARRATIVE
GENERICS AREN’T SAFE
I KNOW A WOMAN WHO HAD A SEIZURE AFTER SWITCHING
SHE’S NOW PARALYZED
AND YOU WANT TO TALK ABOUT ‘SAVING MONEY’?
WHEN DID WE STOP VALUING SAFETY?
THE FDA IS A CORRUPT BUREAUCRACY
THEY LET CHINA MAKE OUR PILLS
YOU WANT TO DIE? KEEP TAKING GENERICS
I’M NOT AFRAID TO SAY IT
THIS IS A MASS MURDER IN PLAIN SIGHT
Matthew Ingersoll
January 8, 2026 AT 15:04That study from Hershman in 2011? I’ve cited it in three medical school lectures.
Adherence jumped from 68% to 73%-that’s not a statistic. That’s 12,000 women in the U.S. alone who didn’t relapse.
And yet, we still have pharmacists handing out branded samples like they’re candy.
It’s not ignorance. It’s profit.
carissa projo
January 8, 2026 AT 16:37There’s a quiet revolution happening here-and most people don’t even notice it.
It’s not in the headlines. It’s not on TV. It’s in the quiet sigh of someone who finally fills their prescription without crying.
It’s in the elderly woman who smiles because she can afford her pills this month.
It’s in the dad who doesn’t have to choose between insulin and his kid’s school trip.
Generics aren’t just medicine.
They’re dignity.
And we owe it to each other to fight for them.
You don’t need to be a doctor or a politician.
You just need to ask.
‘Is there a cheaper option?’
That one question saves lives.
And you? You’re already part of the change.
josue robert figueroa salazar
January 9, 2026 AT 15:47Real talk: the system is rigged.
Generics are cheaper because Big Pharma lets them be.
They own the patents. They own the distribution.
They make billions on brand names.
Then they sell generics at cost to look good.
It’s a scam dressed in a white coat.
And you’re all just cheerleading the illusion.
david jackson
January 10, 2026 AT 18:41Let me tell you what really happened when my cousin switched to generic metformin.
He went from taking it every other day because of the $90 copay… to taking it religiously every morning at 7 a.m., no matter what.
His A1C dropped from 9.1 to 6.4 in four months.
He started hiking again. He took his daughter to Disney. He didn’t miss a single workday.
And then-this is the kicker-he called his doctor and said, ‘Why didn’t you tell me this was an option?’
Because the system doesn’t want you to know.
Because if you knew, you’d stop buying the $150 brand.
And that’s the real reason generics aren’t pushed harder.
Not because they don’t work.
Because they work too well.
And that breaks the profit model.
So they keep you confused. They keep you scared. They keep you paying.
Don’t let them.