How to Build a Personal Medication Safety Plan with Your Care Team
Every year, medication safety plan failures lead to preventable hospital visits, falls, confusion, and even deaths. Most of these aren’t caused by bad doctors or faulty pills. They happen because the system breaks down between appointments - when no one is watching, when labels get faded, when a pill gets mixed up with another, or when a patient forgets to tell their pharmacist about the herbal supplement they started taking. You don’t need to be a medical expert to stop this. You just need a clear, simple plan - and the courage to ask questions.
Start with a Complete List of Everything You Take
- Write down every prescription you’re on - even the ones you only take once a week.
- Include every over-the-counter pill: pain relievers, sleep aids, antacids.
- Don’t forget vitamins, minerals, herbal supplements, or CBD oils. These aren’t harmless. St. John’s Wort can interfere with antidepressants. Ginkgo biloba can thin your blood. Turmeric can affect blood sugar.
- Write down the dose and how often you take it. Example: “Lisinopril 10 mg - one pill daily at breakfast.”
- Include why you take each one. “Metformin for type 2 diabetes.” “Atorvastatin to lower cholesterol.”
- Write down who prescribed it and when you started. “Dr. Patel, Jan 2024.”
Do this now. Don’t wait for your next appointment. Use a notebook, your phone’s notes app, or print a free template from the FDA website. Keep it with you - in your wallet, purse, or phone. This list is your lifeline if you ever end up in the ER.
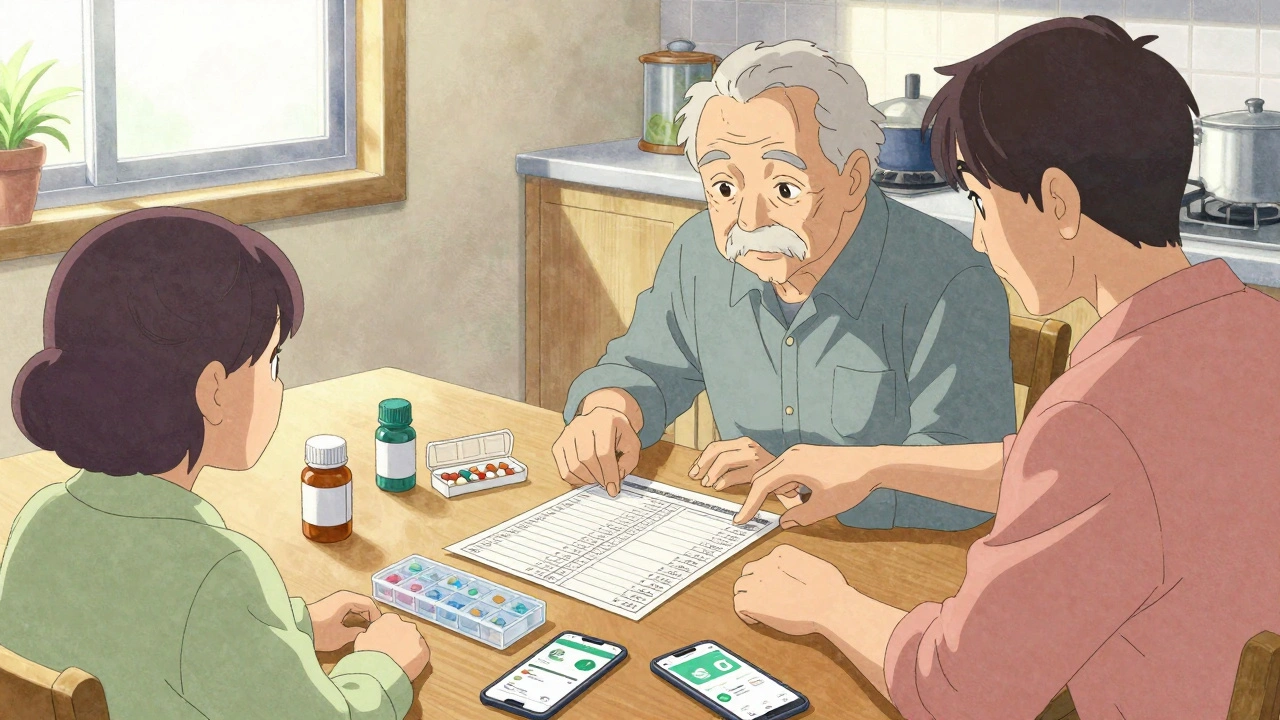
Meet with Your Care Team - Together
Don’t go to your doctor alone if you can help it. Bring a family member, friend, or caregiver. You’ll forget things. They won’t. And they can ask questions you’re too nervous to ask.At the appointment, hand them your list. Say: “I want to make sure all of these are still right for me. Are any of them dangerous together? Are any no longer needed?”
Ask these specific questions:
- “Is this medication still necessary, or can I stop it?”
- “What side effects should I watch for - and what do I do if they happen?”
- “Does this interact with any of my other meds, including supplements?”
- “Is there a cheaper or safer alternative?”
- “Can you write down the instructions in simple words? I don’t want to guess.”
Pharmacists are your secret weapon. Many don’t realize they can answer these questions without a doctor’s note. Walk into the pharmacy with your list. Ask: “Can you check this for interactions?” Most will do it for free.
Label Everything Clearly - No Exceptions
A pill bottle with “Take as needed” and no name on it? That’s a disaster waiting to happen.Here’s how to fix it:
- Use a permanent marker to write your full name on every container - even the little ones.
- Write the medication name clearly: “Metoprolol 25 mg” - not “BP pill.”
- Write the dose and frequency: “Take 1 tablet by mouth at 8 a.m. and 8 p.m.”
- Write the prescribing doctor’s name and phone number.
- For high-risk meds like opioids, blood thinners, or insulin, add a red sticker that says “HIGH ALERT.”
If you use a pill organizer, label each compartment with the day and time. Don’t rely on color-coding alone. If you’re blind, have low vision, or struggle with memory, ask your pharmacist for a talking pill dispenser or large-print labels.
Store Medications Safely - Lock Them Up
Medications aren’t candy. They’re dangerous if taken by the wrong person - or taken by the right person at the wrong time.Keep all pills - even your daily ones - in a locked box or cabinet. Not on the bathroom counter. Not next to your coffee maker. Not in an open drawer. Use a small lockbox from the hardware store, or a medicine lockbox sold at pharmacies.
This is especially critical if:
- You have children or grandchildren visiting.
- You live alone and are at risk of accidental overdose.
- You take painkillers, sedatives, or psychiatric meds.
- You’ve had memory lapses or confusion in the past.
One caregiver on Reddit shared how her mother took a double dose of heart medication because she kept it in an unlabeled bottle next to her bed. She thought it was her blood pressure pill. She ended up in the hospital. A locked box and clear labels would have stopped that.
Use a System to Take Medications Correctly
Your brain isn’t a pharmacy. You’re not supposed to remember 10 pills, 3 times a day, with different rules for each.Use a pill organizer. Buy one with compartments for morning, afternoon, evening, and night. Fill it once a week. Do it on Sunday when you’re calm and have time.
If you’re forgetful, set phone alarms. Name them clearly: “Take Lisinopril - 8 a.m.” Don’t just say “Meds.”
For people with dementia or cognitive decline, use simple language. Write: “This pill is for your heart. Take it with breakfast.” Stick the note to the pill box. Or record a voice message on your tablet: “Hi, it’s time for your blood pressure pill.”
Never skip doses to “save” pills. Never take extra doses if you miss one. Call your doctor or pharmacist instead.
Check In Regularly - Don’t Wait for a Crisis
Medications aren’t set-and-forget. Your body changes. Your health changes. Your other meds change.Set a reminder for every 3 months: “Medication Review.”
At each check-in, ask:
- “Are any of these causing dizziness, confusion, or fatigue?”
- “Have any new symptoms started since I began this med?”
- “Can we remove any pills that aren’t helping?”
- “Has my kidney or liver function changed? Does that affect my doses?”
Many older adults are on 5, 7, even 10 medications. Studies show that 50-60% of adverse drug events come from prescribing and monitoring errors - not from pharmacies or patients. Your care team needs to see you regularly to catch these before they hurt you.
Plan for Emergencies - Before They Happen
If you fall, pass out, or get rushed to the hospital, no one will know what you’re taking unless you’ve prepared.Do this now:
- Keep a printed copy of your medication list in your wallet.
- Give a copy to your main caregiver - spouse, child, neighbor.
- Put a copy in your car glove box.
- Upload a digital version to your phone’s health app or a secure cloud folder.
- Write down your doctor’s name, phone, and the name of your pharmacy.
If you take blood thinners, insulin, or heart meds, consider wearing a medical alert bracelet. It can save your life.

Who Should Manage Your Meds?
If you’re struggling - forgetting doses, mixing pills up, feeling overwhelmed - don’t be proud. Ask for help.Assign a trusted person to manage your medications. It could be your daughter, your neighbor, your home health aide. Give them access to your pill organizer, your list, and your locked box.
They don’t need to be a nurse. They just need to:
- Fill the pill box once a week.
- Check that you’ve taken your meds.
- Call the pharmacy when you’re running low.
- Bring the list to every appointment.
This isn’t about losing independence. It’s about staying safe. And it’s not a sign of weakness - it’s smart planning.
What to Do If Something Feels Wrong
If you feel dizzy after taking a new pill. If you’re confused. If your skin turns yellow. If you’re having trouble breathing. Don’t wait. Don’t think it’s “just aging.”Call your doctor or pharmacist immediately. Say: “I started this new med on [date], and now I feel [symptom]. I’m worried it’s a reaction.”
Keep a journal. Write down:
- What you took
- When you took it
- What you felt
- How long it lasted
This isn’t fluff. It’s data. And it’s the only way your care team can fix the problem.
Medication Safety Isn’t Perfect - But It’s Yours to Control
The system isn’t flawless. Pills get mislabeled. Doctors miss interactions. Pharmacies get busy. But you have more power than you think.You are the only person who knows exactly how you feel after taking each pill. You’re the only one who can spot when something’s off. You’re the only one who can ask the questions no one else will.
Build your plan. Update it. Share it. Stick to it. You’re not just managing pills. You’re protecting your health, your independence, and your future.
What should I do if I miss a dose of my medication?
Never double up unless your doctor or pharmacist tells you to. Call them right away. Some meds, like blood thinners or insulin, can be dangerous if you take too much. Others, like antibiotics, lose effectiveness if you skip doses. Your care team will tell you the safest way to catch up.
Do I need to tell my doctor about vitamins and supplements?
Yes - always. Many people think supplements are harmless, but they can interact badly with prescription drugs. St. John’s Wort can make antidepressants useless. Calcium can block thyroid meds. Garlic or ginseng can thin your blood. Your doctor needs the full picture to keep you safe.
How often should I update my medication list?
Update it every time your meds change - whether you start, stop, or change the dose. At minimum, review it once a year with your doctor. But if you’re on 5 or more medications, review it every 3 months. Your body changes. Your needs change. Your list should too.
Can I use a smartphone app instead of a paper list?
Yes - but don’t rely on it alone. Apps like MyTherapy or Medisafe are helpful for reminders and tracking. But if you’re in an emergency and your phone dies, no one can see your list. Always carry a printed copy. Use the app as a backup, not your only tool.
What if my care team won’t listen to me?
You have the right to be heard. If your doctor dismisses your concerns, ask for a second opinion. Go to a different clinic. See a pharmacist. Bring someone with you to speak for you. Medication safety is not optional. If you feel unsafe, trust your gut. Find someone who will help you stay safe.
Is it okay to throw away old medications?
Never flush them down the toilet or toss them in the trash unless there’s a take-back program. Many pharmacies have medication disposal bins. If not, mix pills with coffee grounds or cat litter in a sealed bag before throwing them away. This keeps them from being picked up by kids or pets. Always remove personal info from the bottle first.

Rebecca Braatz
December 5, 2025 AT 07:49Just printed out my med list and stuck it in my wallet today-finally. Been putting this off for months. My grandma nearly ended up in the ER last year because she mixed up her blood pressure pill with her calcium. Don’t be like me. Do it now. No excuses.
Martyn Stuart
December 6, 2025 AT 06:03Agreed-labeling is non-negotiable. I’ve seen too many cases where ‘BP pill’ led to confusion, and someone took the wrong thing. Use a permanent marker. Write the full name, dose, frequency, and prescriber. And for heaven’s sake, don’t rely on color-coding alone-colorblind people exist, and memory fails. Also, pharmacists are underutilized. Walk in with your list. They’ll check interactions for free. No appointment needed.
Shofner Lehto
December 7, 2025 AT 05:33Lock your meds. Seriously. I used to keep my painkillers on the nightstand. My nephew, age 7, found them during a visit. He thought they were candy. Thank God he only swallowed one. Now everything’s in a locked box on the top shelf. No exceptions. Even my daily vitamins. If it’s not food, it doesn’t belong where a kid can reach it.
Emmanuel Peter
December 8, 2025 AT 14:00Everyone’s acting like this is revolutionary. Newsflash: this is basic hygiene. If you’re over 65 and on more than three meds, you’re already in danger. The system is designed to fail you. Doctors don’t have time. Pharmacies are understaffed. You think your doctor remembers every pill you’re on? They’re juggling 30 patients an hour. You’re the only one who can save yourself. Stop waiting for permission. Start acting like your life depends on it-because it does.
Ashley Elliott
December 9, 2025 AT 01:49I’ve been using the MyTherapy app for a year, and it’s great for reminders-but I still carry the printed list in my purse. My mom had a stroke last winter, and the ER staff couldn’t access her phone. They had to call my sister to get the list. Don’t put all your eggs in one basket. Digital is convenient. Paper is reliable. Use both.
Joe Lam
December 9, 2025 AT 16:21People treat supplements like they’re harmless tea. St. John’s Wort, ginkgo, turmeric-these aren’t ‘natural wellness products.’ They’re active pharmaceutical compounds with documented interactions. If you’re on an SSRI and take St. John’s Wort, you could develop serotonin syndrome and die. This isn’t ‘being cautious.’ This is basic pharmacology. If you don’t know this, you shouldn’t be self-medicating.
Rachel Bonaparte
December 10, 2025 AT 07:56Let’s be real-this whole system is rigged. Big Pharma doesn’t want you to know how dangerous polypharmacy is. They profit from you taking more pills, not fewer. Your doctor gets paid for prescribing, not for deprescribing. And don’t get me started on how the FDA approves drugs with minimal long-term data. You think your ‘blood pressure pill’ was tested for 20 years of use? Nope. Three months. That’s why you get side effects. They’re not side effects-they’re warnings. And nobody’s telling you the truth. You’re being experimented on, and you’re the one holding the pill bottle.
Scott van Haastrecht
December 10, 2025 AT 09:23I’ve seen this before. A woman in my building took her husband’s blood thinner because she thought it was her vitamin. He died. She didn’t even realize until the funeral. No labels. No lockbox. No list. Just a drawer full of mystery pills. This isn’t about ‘safety.’ This is about accountability. And if you’re not willing to do the work, you’re putting your life-and others’ lives-at risk. This isn’t a suggestion. It’s a survival protocol.
Chase Brittingham
December 11, 2025 AT 18:38My dad used to forget if he took his meds. I started filling his pill box every Sunday. He’d get mad at first-said he didn’t need help. But after he missed a dose and got dizzy walking to the mailbox, he stopped arguing. Now he says, ‘Thanks for keeping me alive.’ It’s not about control. It’s about love. You don’t have to do it alone. Ask someone. Let someone help. That’s not weakness. That’s wisdom.
Bill Wolfe
December 13, 2025 AT 11:59Let me be blunt: if you’re not using a locked box, labeling every container, and reviewing your meds every 90 days, you’re not just irresponsible-you’re a liability. And if you’re using a smartphone app as your primary system? You’re one dead battery away from disaster. Real adults don’t rely on tech they can’t control. Real adults have paper. Real adults have backups. Real adults don’t wait for a crisis to start being responsible. And if you’re still taking ‘natural’ supplements without checking interactions? You’re one step away from an ICU. This isn’t opinion. It’s fact. And you’re not helping anyone by ignoring it.