How to Check Active Ingredients to Prevent Double Dosing in Children

Every year, thousands of children end up in emergency rooms because their parents gave them too much of the same medicine-without even realizing it. It’s not because they’re careless. It’s because they didn’t know what to look for. Active ingredients are the hidden danger in most children’s medicines. Two different-looking bottles can contain the exact same chemical, and giving both can be deadly.
Why Double Dosing Happens
Parents aren’t trying to hurt their kids. They’re trying to help. A child has a fever, so they give acetaminophen. Later, the child starts coughing, so they grab a cold medicine from the cabinet. It seems harmless. But if that cold medicine also contains acetaminophen, they’ve just doubled the dose. And that’s when things go wrong. The problem exploded after the FDA warned against giving cough and cold medicines to kids under 2 in 2007. Parents started mixing separate products-fever reducers, cough syrups, antihistamines-thinking they were being smarter. But they didn’t realize most of these products share the same active ingredients. In fact, 89% of multi-symptom cold medicines contain acetaminophen. And 73% of parents can’t tell when two different brands have the same ingredient inside. Children are especially vulnerable. Their bodies process medicine differently. A dose that’s safe for a 40-pound child could be toxic for a 20-pound child. And for kids under 5, even a 10% overdose can double the risk of serious side effects. The most common culprit? Acetaminophen. It’s in over 600 products-from Tylenol to NyQuil to Vicks DayQuil. Too much can cause liver failure. In children under 6, acetaminophen overdose is responsible for 45% of all acute liver failure cases.Common Active Ingredients to Watch For
You don’t need to memorize every chemical name. Just learn these five, and you’ll avoid 90% of double dosing risks:- Acetaminophen (also called paracetamol, APAP, or N-acetyl-p-aminophenol) - used for fever and pain. Found in Tylenol, Panadol, NyQuil, Theraflu, Sudafed PE, and many cough syrups.
- Ibuprofen - used for fever and pain. Found in Advil, Motrin, and some cold formulas.
- Diphenhydramine - an antihistamine used for allergies and sleep. Found in Benadryl, Children’s NyQuil, and some cough syrups.
- Pseudoephedrine - a decongestant. Found in Sudafed, Claritin-D, and many multi-symptom cold meds.
- Phenylephrine - another decongestant, often used instead of pseudoephedrine. Found in Children’s Sudafed, Mucinex D, and DayQuil.
How to Check Before Giving Any Medicine
Here’s a simple, proven method that works:- Write it down. Keep a list of every medicine in your home. Include the brand name, active ingredient, concentration (like 160mg/5mL), and why you use it. Update it every time you buy something new.
- Check before you give. Before giving any medicine, ask: “Does this have the same active ingredient as something I already gave today?” If yes, don’t give it.
- Use the right tool. Never use a kitchen spoon. Always use the measuring cup, syringe, or dropper that came with the medicine. Household spoons can be off by up to 200%. A teaspoon might hold 2.5mL or 7.5mL-it’s not reliable.
- One person gives the meds. Designate one parent or caregiver to handle all doses. This cuts down on miscommunication, which causes 38% of double dosing errors.
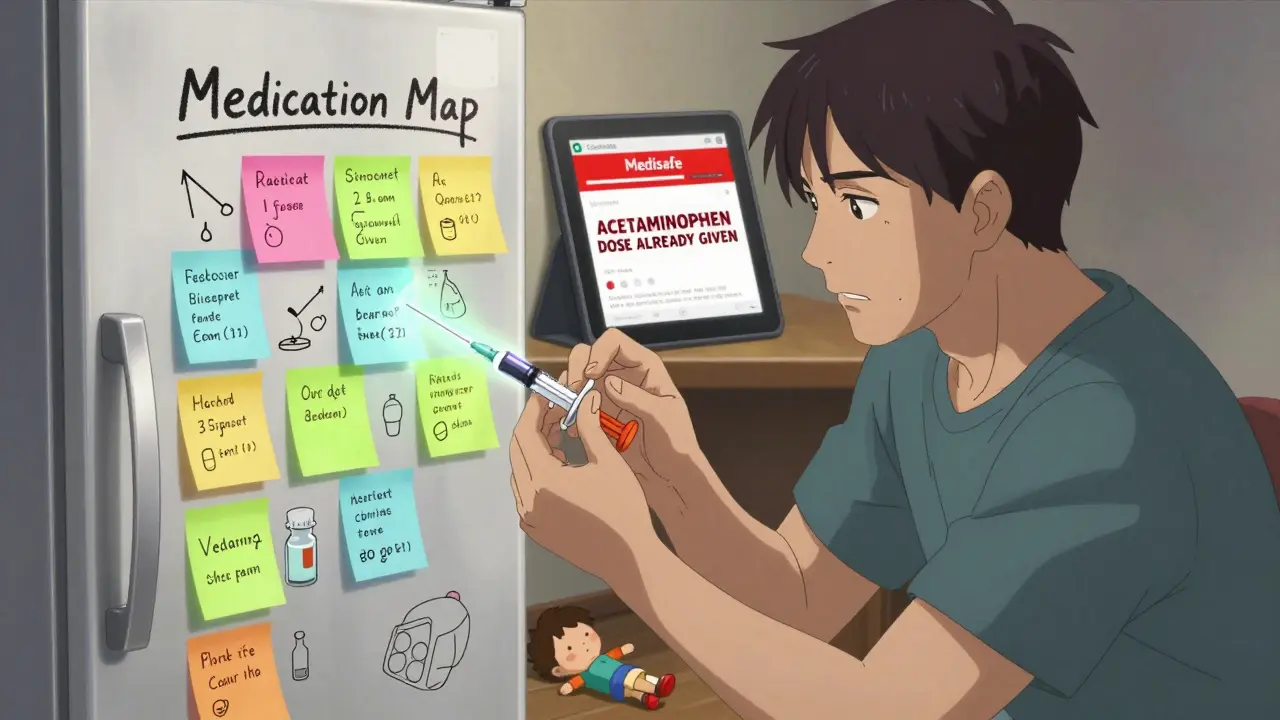
- Use a timer or app. Apps like Medisafe or Round Health can remind you when the last dose was given and warn you if you’re about to repeat an ingredient. Even if you don’t use an app, write the time and medicine on a sticky note next to the cabinet.
What to Do If You Think You’ve Double Dosed
If you realize you gave your child two doses of the same medicine-or two medicines with the same active ingredient-don’t panic. But don’t wait either.- Call Poison Control immediately. In the U.S., it’s 1-800-222-1222. They’re free, confidential, and available 24/7. Don’t wait for symptoms. Don’t Google it. Call.
- Have the medicine bottle ready. When you call, have the label in hand. Tell them the name of the medicine, the active ingredient, how much was given, and when.
- Don’t induce vomiting. Unless Poison Control tells you to, don’t try to make your child throw up. It can make things worse.
- Watch for symptoms. For acetaminophen: nausea, vomiting, loss of appetite, yellow skin or eyes. For diphenhydramine: extreme drowsiness, confusion, fast heartbeat, trouble breathing. For ibuprofen: stomach pain, vomiting, dizziness. If any of these appear, go to the ER.
What’s Changing to Help Parents
The system is starting to catch up. In January 2024, the American Academy of Pediatrics launched the “Know Your Ingredients” campaign, pushing for standardized icons on medicine packaging. By December 2025, the FDA will require all children’s OTC medicines to list active ingredients in bold, standardized format. No more hiding them in tiny print. Some companies are adding QR codes to bottles. Scan it, and you’ll see a breakdown of all active ingredients and what they’re used for. Johnson & Johnson and Procter & Gamble have rolled this out on 45% of their pediatric products. Amazon Pharmacy’s new “MedCheck” feature scans your order and flags potential overlaps. In its first six months, it prevented an estimated 12,000 double dosing incidents. But the most powerful tool is still you. Technology helps. But checking the label? That’s something you can do right now. No app required. No cost. Just attention.
What Not to Do
Avoid these common mistakes:- Don’t alternate acetaminophen and ibuprofen for fever. The American Academy of Family Physicians says this increases double dosing risk by 47%. Stick to one, and use it correctly.
- Don’t assume “children’s” means safer. Children’s Tylenol and Children’s NyQuil both have acetaminophen. One is labeled for fever. The other for colds. Same ingredient. Same risk.
- Don’t trust flavor. A parent once told a pharmacist they gave more of the strawberry-flavored medicine because “it’s weaker.” It wasn’t. The concentration was identical.
- Don’t use expired medicine. Old meds can lose potency-or become unstable. Toss anything past its date.
Real Stories, Real Lessons
One dad on BabyCenter created a “medication map” on his fridge. He listed every medicine in the house with its active ingredient. He showed it to his wife, his sister, his mom. After six months, his family had zero dosing errors. Zero. He said it took 10 minutes to make-and saved them from a possible trip to the ER. Another parent gave her 18-month-old both a fever reducer and a cold syrup. She didn’t realize both had acetaminophen. Her child got sick. They went to the hospital. She learned the hard way. Now, she keeps a printed list in her wallet. “I don’t trust my memory,” she says. “I trust the paper.”Final Rule: When in Doubt, Don’t Give It
If you’re unsure whether two medicines have the same active ingredient, don’t give the second one. Call your pharmacist. Call Poison Control. Wait until you’re sure. It’s better to wait an hour than risk a liver injury, a seizure, or worse. Double dosing isn’t about being a bad parent. It’s about being overwhelmed. There are too many products. Too many names. Too many labels. But you don’t need to know everything. You just need to know how to check. Start today. Look at the medicine cabinet. Pick one bottle. Read the Active Ingredients line. Write it down. Do it for every one. In 20 minutes, you’ll know more than 70% of parents do. And your child will be safer because of it.How do I know if two children’s medicines have the same active ingredient?
Look at the “Active Ingredients” section on the Drug Facts label. Ignore the brand name, flavor, or packaging. Compare the exact chemical names. Acetaminophen, ibuprofen, diphenhydramine, pseudoephedrine, and phenylephrine are the top five to watch. If they match, don’t give both.
Can I give my child acetaminophen and ibuprofen together?
It’s not recommended for children under 3. Alternating them increases the risk of accidental double dosing by 47%. Stick to one, and use it as directed. If the fever doesn’t break, talk to your pediatrician-not your medicine cabinet.
Is it safe to use a kitchen spoon to measure liquid medicine?
No. Household spoons vary wildly in size-from 2.5mL to 7.5mL. The FDA says this leads to triple dosing in some cases. Always use the measuring device that came with the medicine. If you lost it, ask your pharmacist for a new one-they’ll give it to you for free.
What should I do if I think my child got too much medicine?
Call Poison Control at 1-800-222-1222 right away. Don’t wait for symptoms. Have the medicine bottle ready. Tell them the name, active ingredient, amount given, and time. Do not induce vomiting unless instructed. If your child is having trouble breathing, turning blue, or is unresponsive, call 911.
Why do some medicines list “paracetamol” instead of “acetaminophen”?
It’s the same thing. Acetaminophen is the name used in the U.S. Paracetamol is used in Europe, Australia, and many other countries. APAP and N-acetyl-p-aminophenol are also the same. If you see any of these, treat them as identical. Don’t assume they’re different.
Are there apps that can help prevent double dosing?
Yes. Apps like Medisafe and Round Health track doses and warn you if you’re about to repeat an active ingredient. They’re not perfect, but they reduce double dosing risk by 52% when used consistently. Still, they’re a tool-not a replacement for checking labels yourself.
How can I teach my partner or babysitter to avoid double dosing?
Create a simple one-page list: Medicine Name | Active Ingredient | Dose | Time Given. Keep it on the fridge or in your phone. Show them how to check the label before giving anything. Say: “If it has the same name as something already given, don’t give it.” Make it a habit, not a guess.

Alana Koerts
December 18, 2025 AT 11:02Acetaminophen is in everything. Seriously. I checked my kid's cough syrup last week-same as the fever med. I almost killed him with my ignorance. Don't be like me.
Dominic Suyo
December 19, 2025 AT 14:39Let’s be real-this isn’t about parenting. It’s about pharmaceutical companies designing products to maximize liability while minimizing labeling clarity. They want you to mess up. Then they profit off the ER visits. The FDA’s ‘standardized icons’? Too little, too late. The real fix? Ban multi-symptom pediatric meds entirely. Or at least make them require a damn prescription.
And don’t get me started on phenylephrine. It’s a placebo disguised as a decongestant. But hey, at least it’s in the label. Unlike the 37 other hidden antihistamines in ‘natural’ kids’ formulas.
Kevin Motta Top
December 20, 2025 AT 07:28My wife and I made a laminated card with the top 5 ingredients. We keep it taped to the medicine cabinet. Takes 5 seconds. Saved us twice. Simple wins.
Alisa Silvia Bila
December 21, 2025 AT 22:19I used to think I was careful. Then I gave my 2-year-old Tylenol and a cold syrup that had APAP. I didn’t even know APAP meant acetaminophen. I felt like an idiot. Now I always check the label like it’s a bomb defusal manual. No shame in being extra.
Marsha Jentzsch
December 23, 2025 AT 12:37Oh my GOD, I just checked my cabinet-TWO bottles of children’s NyQuil! I thought one was for day and one was for night! I didn’t even realize they both had diphenhydramine! I’m so stupid. I’m calling Poison Control right now. I feel sick just thinking about it. Why does no one tell you this?!!
Carolyn Benson
December 24, 2025 AT 03:09It’s not about checking labels. It’s about systemic failure. We’ve outsourced parental responsibility to corporations who profit from confusion. The real crime isn’t the overdose-it’s the fact that we’ve normalized this. Parents aren’t negligent. We’re weaponized by capitalism. You think you’re helping? You’re just another cog in the pharmaceutical machine. Wake up.
And yes, I’ve read the FDA guidelines. I’ve read the AAP white papers. I’ve read the 2023 study. You’re still reading this because you haven’t done the work. Go check your cabinet. Now.
Aadil Munshi
December 25, 2025 AT 09:32Love how you broke this down. I’m from India, and here, parents mix Ayurvedic syrups with OTC meds all the time. No one checks ingredients. I showed my sister-in-law the list-she cried. Said she’d given her baby two meds with paracetamol last month. We’re all just trying to do better. Thanks for the clarity.
Frank Drewery
December 25, 2025 AT 18:56This is the kind of post that makes me believe people still care. I’ve been a nurse for 18 years. I’ve seen the aftermath. I’ve held babies who didn’t make it because someone didn’t know what ‘APAP’ meant. Please, if you read one thing today-read the label. It’s not complicated. Just slow down. You’ve got this.
mary lizardo
December 26, 2025 AT 15:23While the intent of this post is commendable, the grammatical inconsistencies-particularly the inconsistent use of serial commas and the erratic capitalization of ‘Active Ingredients’-undermine its credibility. Furthermore, the reliance on anecdotal Reddit stories as evidence is methodologically unsound. A properly sourced, peer-reviewed meta-analysis would have been more appropriate. That said, the core message remains valid: label literacy is non-negotiable.