How to Ensure Medication Safety in Hospitals and Clinics

Every year, hundreds of thousands of patients in U.S. hospitals suffer harm from medication errors that never should have happened. These aren’t rare accidents-they’re preventable failures in systems that are supposed to keep people safe. A patient gets the wrong dose of insulin. A nurse administers methotrexate daily instead of weekly. An elderly person leaves the hospital with conflicting instructions for their blood thinner. These aren’t just mistakes. They’re symptoms of broken processes.
Why Medication Safety Isn’t Just About Being Careful
Medication safety isn’t about trusting staff to be perfect. It’s about designing systems that make it nearly impossible to get it wrong-even when people are tired, rushed, or distracted. The Institute of Medicine’s landmark 1999 report, To Err is Human, revealed that up to 98,000 people die annually in U.S. hospitals from preventable errors, with medication mistakes accounting for about 7,000 of those deaths. That’s more than car crashes. More than breast cancer. And most of it? Avoidable.Today, the cost of these errors isn’t just measured in lives lost. It’s $21 billion a year in extra healthcare spending. That’s money spent on extended hospital stays, emergency treatments, and legal settlements-all because a pill was given at the wrong time, in the wrong way, or to the wrong person.
The Core of Medication Safety: High-Alert Medications
Not all medications carry the same risk. Some are so dangerous that even a small mistake can kill. These are called high-alert medications. The Institute for Safe Medication Practices (ISMP) maintains the official list, and it includes drugs like insulin, opioids, anticoagulants, and intravenous potassium chloride. One wrong dose of insulin can send a patient into a coma. A single misstep with an opioid can stop someone’s breathing.ASHP guidelines say these drugs need special safeguards: independent double-checks by two licensed staff, standardized concentrations (no more custom mixes), and automated dose range alerts in electronic systems. But here’s the catch: many hospitals still don’t follow all of these rules. A 2021 survey found that 63% of hospitals struggled to build hard stops into their electronic health records for high-alert meds because their software vendors wouldn’t let them.
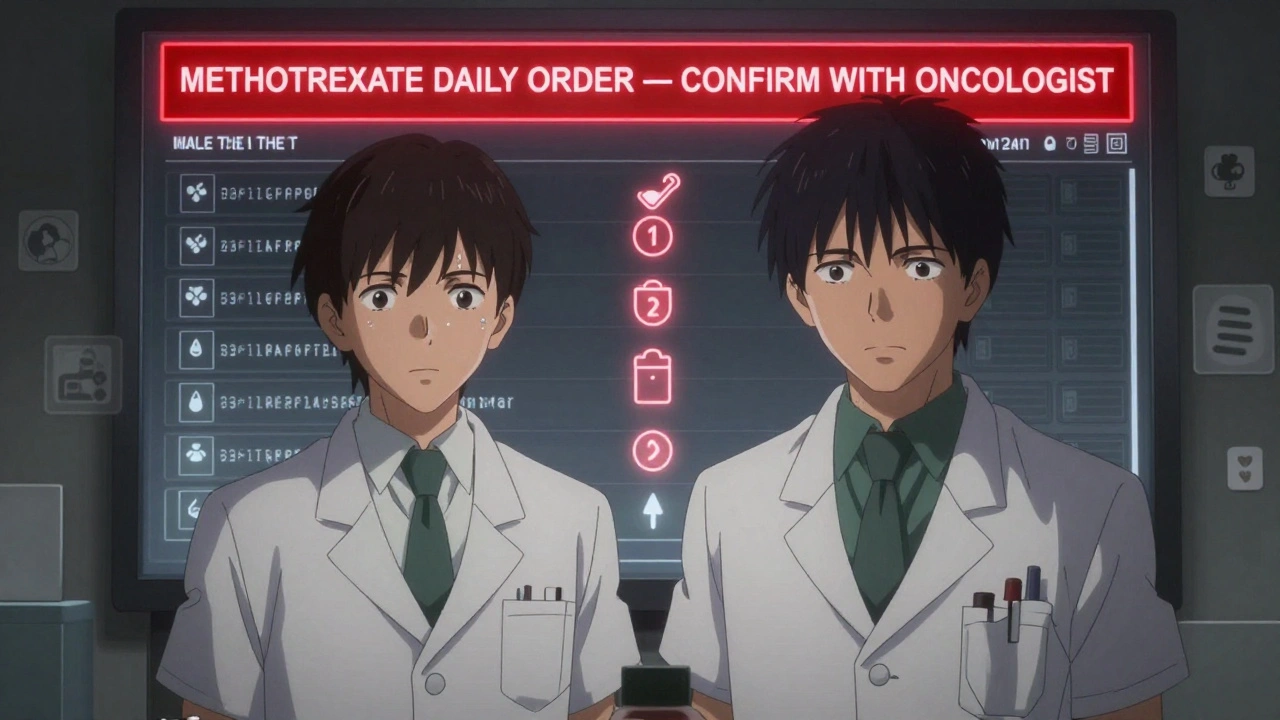
The Methotrexate Case: One Rule That Saved Lives
One of the most powerful examples of medication safety in action is the fix for methotrexate. This drug is used for cancer, autoimmune diseases, and sometimes ectopic pregnancies. But it’s deadly if given daily instead of weekly. For years, patients died because someone ordered it as a daily dose-and no one caught it.In 2020, ISMP made it mandatory: hospitals must set their electronic systems to default to weekly dosing. If a provider tries to order it daily, the system locks up and demands a second confirmation from an oncologist. That’s called a hard stop. Since then, an estimated 1,200 serious errors have been prevented each year, according to Dr. Robert Wachter of UCSF.
But it’s not just about technology. Patients need to understand it too. ISMP requires hospitals to give both written and verbal discharge instructions for methotrexate. Patients are told: “Take this once a week. Not every day. If you’re unsure, call your doctor.” One pharmacy director in a Midwest hospital said the hard stop caught three near-misses in the first month alone.
Barcode Scanning and the Right Patient Check
Another proven tool? Barcode medication administration (BCMA). Nurses scan the patient’s wristband, then scan the medication. The system checks: Is this the right drug? Right dose? Right time? Right patient? If not, it won’t allow the dose to be given.Studies show hospitals using full BCMA systems see 55% fewer serious medication errors. But adoption isn’t universal. Only 54% of small hospitals (under 100 beds) use it, compared to 89% of large ones. Why? Cost. Training. Legacy systems. Some nurses still rely on manual checks because the barcode scanner isn’t working-or they’re too busy to use it.
Patients notice the difference. A 2022 survey by the National Council on Aging found that 68% of adults over 65 feel safer when nurses verify their name, birth date, and wristband before giving any medication. That’s not just protocol. It’s trust.
Medication Reconciliation: The Missing Link
One of the biggest gaps in medication safety happens when patients move between settings. A person goes from the ER to the floor. From hospital to rehab. From clinic to home. Each time, their medication list gets rewritten-sometimes incorrectly.Medication reconciliation is the process of comparing what a patient should be taking with what they are taking. It’s not optional. The Joint Commission requires it. But too often, it’s done poorly. A nurse asks, “What meds are you on?” The patient says, “I take a blue pill and a white one.” The nurse writes down “ibuprofen and aspirin.” Turns out, the blue pill was a blood thinner, and the white one was a seizure drug. Neither was documented in the hospital system.
Effective reconciliation requires pharmacists-not just nurses-to lead the process. It needs access to outside records, clear communication with primary care providers, and a standardized form that doesn’t get lost in paperwork.
Why Some Hospitals Succeed-and Others Don’t
Not all hospitals follow the same rules. ISMP’s Targeted Medication Safety Best Practices are detailed, specific, and evidence-based. But they’re also demanding. Implementing them costs an average of $285,000 per hospital in tech upgrades and training. A 2022 ECRI Institute study found only 42% of community hospitals fully adopted all 19 ISMP practices. Academic medical centers? 78% did.Meanwhile, the Joint Commission’s National Patient Safety Goals are broader and easier to comply with-but less effective. A 2021 study in the Journal of Patient Safety showed hospitals using ISMP’s full set had 37% fewer preventable harm incidents than those relying only on Joint Commission standards.
But here’s the real problem: too many hospitals try to follow both. Staff get confused. They’re told to follow one rule on Monday, another on Tuesday. Dr. David Bates of Brigham and Women’s Hospital calls this “implementation fatigue.” Frontline workers aren’t resistant to safety-they’re exhausted by conflicting instructions.
The Human Side: Nurses, Pharmacists, and Patients
Medication safety isn’t just about software. It’s about people. A nurse in a rural hospital posted on the American Nurses Association forum: “The requirement for written and verbal methotrexate instructions created bottlenecks during staffing shortages.” She wasn’t against safety. She was overwhelmed.On the flip side, a Reddit post from an ICU nurse described how inconsistent high-alert protocols led to a patient nearly dying from a neuromuscular blocker error. Multiple safety layers were in place-but none were activated because no one knew which one to follow.
Patients are part of the solution too. Pilot programs at Mayo Clinic and Johns Hopkins now ask patients to review their own medication lists before discharge. When patients caught errors, error detection improved by 32%. That’s not just patient empowerment. It’s a safety net.
What’s Next? AI, Regulation, and Outpatient Safety
The future of medication safety is here-and it’s changing fast. By 2025, Gartner predicts 75% of U.S. hospitals will use AI to detect medication errors in real time. Right now, only 22% do. These systems can flag a double dose of warfarin before it’s given. They can spot a drug interaction a human might miss.The FDA is also stepping up. New labeling rules for high-concentration electrolytes go into effect by the end of 2024. Compounded sterile preparations now have stricter standards after a 2022 fungal meningitis outbreak killed dozens.
But the biggest shift? Outpatient safety. Medication errors in clinics and doctor’s offices have jumped 47% since 2018. ISMP is working on expanding its best practices to include ambulatory care in the 2024-2025 update. That’s critical. More people are getting prescriptions from clinics than hospitals. And many of them don’t have pharmacists on-site.
What You Can Do-Even If You’re Not a Doctor
You don’t need to be a nurse or pharmacist to help prevent medication errors. Here’s how:- Keep a current, written list of every medication you take-including doses and why you take them.
- Ask: “Is this the right drug for me? Is this the right dose? What side effects should I watch for?”
- Double-check your discharge papers. Do they match what your doctor told you?
- If you’re giving meds to a loved one, ask the pharmacist to explain the schedule. Write it down.
- Speak up if something looks wrong. A wrong pill color? A different name on the bottle? Say something.
Medication safety isn’t a department. It’s a culture. And it only works when everyone-from the CEO to the patient-takes responsibility.

Scott Butler
December 13, 2025 AT 01:14Let’s be real-this whole medication safety thing is just government overreach dressed up as compassion. We used to trust doctors and nurses to do their jobs without 17 layers of barcode scanners and AI babysitting. Now we’re treating adults like toddlers who can’t read a pill bottle. The real problem? Too many people don’t take responsibility for their own meds. Stop blaming the system and start blaming the idiots who take insulin daily because they ‘forgot’ the instructions.
Emma Sbarge
December 14, 2025 AT 12:48As someone who works in hospital admin, I’ve seen the chaos firsthand. The ISMP guidelines are solid-but implementation is a nightmare. Nurses are stretched thin, EHR vendors are profit-driven, and compliance checks turn into performative rituals. We had a nurse miss a double-check because she was filling out 3 different audit forms while holding a dying patient’s hand. Systems should serve people, not the other way around.
Ronan Lansbury
December 14, 2025 AT 22:47Of course the system is broken. Who do you think controls the EHR vendors? Big Pharma. They don’t want hard stops on high-alert meds because it cuts into their profit margins. The FDA’s new labeling rules? A distraction. The real story is the 2021 data leak from Epic that showed they were selling patient dosing patterns to drug companies. They don’t care if you live or die-they care if your insurance pays for the next round of opioids.
Jennifer Taylor
December 16, 2025 AT 09:01OMG I CANNOT BELIEVE THIS IS STILL HAPPENING 😭 I had my grandma almost die from a blood thinner error because the hospital ‘forgot’ to reconcile her meds. She was on warfarin for 12 years, and they gave her a new prescription with NO REFERENCE. I screamed at the nurse, I called the CEO, I posted on TikTok-it went viral. Now they have a ‘patient advocate’ on every floor. But only because I cried on national news. This isn’t healthcare. It’s a horror show.
Rawlson King
December 17, 2025 AT 20:32Barcodes and AI won’t fix human negligence. The real issue is that hospitals hire underpaid, overworked staff and then punish them when the system fails. You want safety? Pay nurses a living wage. Stop outsourcing pharmacy services to third-party corporations that cut corners. Stop treating healthcare like a startup with a ‘move fast and break things’ mentality. The tech is fine. The culture is toxic.
Michael Gardner
December 18, 2025 AT 06:40Actually, the methotrexate hard stop is a terrible idea. What if someone needs daily dosing for a rare cancer? Now they have to jump through hoops just to get life-saving treatment. Safety protocols shouldn’t assume the worst about clinicians-they should empower them with better tools, not lock them out. This is bureaucracy masquerading as innovation.
Willie Onst
December 19, 2025 AT 18:32Man, I love how this post doesn’t just throw tech at the problem. It’s about people. My aunt was in the hospital last year, and the pharmacist actually sat down with her for 20 minutes, wrote out her meds in big letters, and drew little icons for morning/night. She said it was the first time she felt like someone actually cared. That’s the stuff that saves lives-not software. Just human kindness and clarity.
Shelby Ume
December 20, 2025 AT 06:15Medication reconciliation is not optional. It is a non-negotiable standard of care. Yet, in many community hospitals, it is performed by a nursing assistant with no formal pharmacology training, using a clipboard from 2007. The Joint Commission mandates it, but provides no funding. We cannot continue to rely on goodwill and overtime to fulfill foundational patient safety obligations. Leadership must prioritize funding, training, and accountability-or we will keep burying patients who never should have died.
Jade Hovet
December 21, 2025 AT 05:22THIS. IS. EVERYTHING. 🙌 I’m a pharmacy tech and I’ve seen the same errors over and over-same names, same meds, same mistakes. But when we started using color-coded pill bottles + voice reminders for seniors? Error rates dropped 40%. Also, patients LOVE it when you say ‘Hey, I know this looks weird but your pill is blue now because the generic changed!’ Just talk to people. 😊❤️
John Fred
December 23, 2025 AT 01:21Let’s talk about the real ROI: implementing full BCMA + AI-driven decision support reduces preventable ADEs by 62% (per JAMA 2023). The $285k investment? Paid for itself in 11 months via reduced readmissions and malpractice claims. The problem isn’t cost-it’s leadership inertia. Hospitals still think ‘safety’ is a compliance checkbox, not a value driver. Time to stop treating patient safety like a cost center and start treating it like the core business function it is.