How to Interpret Risk vs. Benefit in FDA Safety Announcements
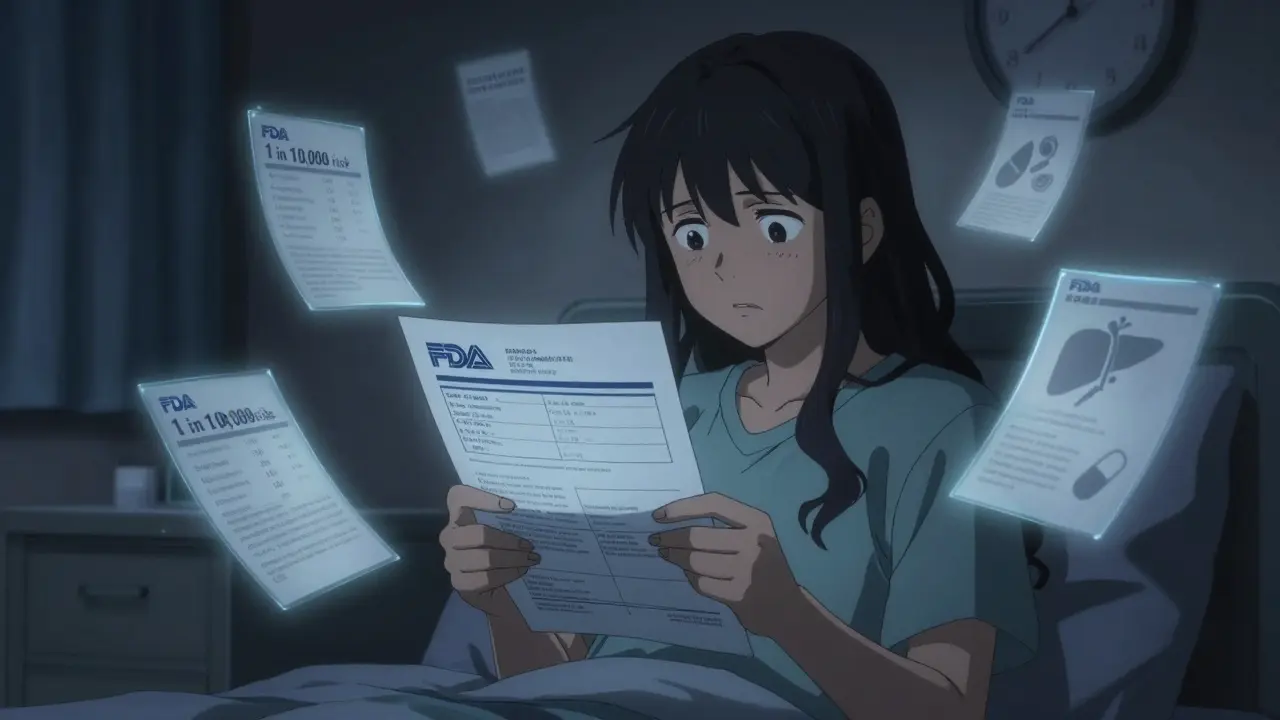
When you see an FDA safety announcement about a medication you or someone you care about is taking, it’s natural to feel alarmed. The headline might say something like, "FDA warns of possible link between Drug X and rare heart condition." Your first thought? Should I stop taking this? But here’s the truth most people miss: an FDA safety alert is not a warning to stop. It’s a signal to pause, dig deeper, and understand the real balance between what the drug does for you - and what it might do to you.
What FDA Safety Announcements Actually Mean
The FDA doesn’t issue these alerts because a drug is dangerous. They issue them because something new showed up in the data - something that wasn’t clear during clinical trials. Clinical trials involve thousands of people, maybe tens of thousands. But once a drug is approved and millions start taking it, rare side effects start to appear. That’s not a failure of the system. That’s how it’s supposed to work. The FDA uses the FDA Adverse Event Reporting System (FAERS), which collects over 1.2 million reports every year from doctors, patients, and drug companies. These reports are raw data - not proof. A report says, "Patient took Drug X and had a stroke." But did the drug cause it? Or was the patient already at high risk? The FDA doesn’t know yet. That’s why they call these early findings "potential signals." Only after reviewing dozens, sometimes hundreds, of similar reports, and comparing them to background rates in the general population, do they determine if it’s a real risk. The key phrase in every FDA alert: "This does not mean the FDA has determined that the drug causes the risk." That’s not legal jargon. It’s scientific honesty.The Difference Between an Adverse Event and an Adverse Drug Reaction
Not every bad thing that happens after taking a drug is caused by the drug. That’s the first rule of interpreting these alerts. - An adverse event is any unwanted medical occurrence after taking a drug - whether it’s related to the drug or not. Headache, nausea, dizziness, even a car accident after taking a sleep aid - all count as adverse events. - An adverse drug reaction is when there’s a reasonable possibility the drug caused the problem. That’s the real concern. The FDA’s job is to separate noise from signal. For example, if 1 in 10,000 people on a new diabetes drug develop a rare liver issue, and only 1 in 100,000 people not on the drug develop it, that’s a signal worth investigating. But if the rate is the same in both groups? It’s likely coincidence.How to Read an FDA Drug Safety Communication
Not all FDA alerts are created equal. Here’s how to quickly sort them:- Look for the word "potential signal" - This means the FDA has noticed a pattern but hasn’t confirmed causation. Don’t panic. Do investigate.
- Look for "confirmed risk" - This means the FDA has enough evidence to say the drug likely causes the problem. Labeling changes or REMS (Risk Evaluation and Mitigation Strategies) usually follow.
- Check if they give numbers - The best alerts say things like, "The risk of this rare condition is estimated at 0.3 cases per 1,000 patients per year." That’s actionable. Vague alerts like "may increase risk" are frustrating - and common.
- Find the benefit context - Was this drug approved for a life-threatening condition? If yes, a higher risk might still be acceptable. A drug for acne? A 1 in 500 risk of liver damage is a big deal.

Ask These Five Questions Before You Act
When you see an alert, don’t rush. Ask yourself:- Is this risk serious? The FDA defines serious as: death, life-threatening, hospitalization, permanent disability, or congenital anomaly. If the risk isn’t serious, the benefit-risk balance is likely still positive.
- How common is it? A 1 in 100,000 risk is tiny. A 1 in 1,000 risk is worth discussing with your doctor.
- Are there alternatives? If this is your only effective treatment for a chronic condition, stopping might be riskier than staying on it.
- Do I have risk factors? Some risks only apply to certain people - older adults, pregnant women, those with kidney disease. Are you in that group?
- Has the FDA changed the label? If the prescribing information now includes a new warning, that’s a formal red flag. If not, the alert is still under review.
Why the FDA’s System Is Flawed - But Still Essential
Critics say the FDA’s alerts are too vague. They’re right. Many don’t include absolute risk numbers. Some make patients terrified of medications that are still safe for most people. The 2021 alert about menstrual changes and COVID-19 vaccines caused widespread confusion - even though later data showed no causal link. But here’s what critics ignore: without this system, dangerous drugs would stay on the market. Thalidomide in the 1950s killed thousands of babies because no one was watching. Today, the FDA catches problems like the increased risk of Fournier’s gangrene with SGLT2 inhibitors - a rare but deadly infection - before it becomes a national crisis. The system isn’t perfect. But it’s the best we have. And it’s getting better. In 2024, the FDA finalized new guidance requiring all safety communications to include six key elements: condition severity, treatment alternatives, benefit size, risk frequency, risk management options, and patient input. By 2025, they’ll start using standardized risk formats - meaning you’ll see numbers like "1 in 1,000" instead of "may increase risk."
What You Should Do Right Now
If you’re on a medication and see a new FDA alert:- Don’t stop taking it unless your doctor tells you to.
- Don’t panic. Read the full alert on the FDA’s website - not just the headline.
- Check if the drug’s prescribing information (the "package insert") has been updated. That’s the real signal.
- Call your doctor. Say: "I saw an FDA alert about [drug name]. Can you help me understand if this affects me?"
- If you’re a patient, report any side effects to the FDA through MedWatch. Your report helps them see patterns.
Real-World Example: SGLT2 Inhibitors and Fournier’s Gangrene
In 2022, the FDA issued a safety alert about a rare but deadly infection called Fournier’s gangrene linked to diabetes drugs like Jardiance and Farxiga. The alert didn’t say, "Stop taking these drugs." It said: "The estimated incidence is 0.2 cases per 1,000 patient-years compared to 0.06 in non-users." That’s a 3.3-fold increase - but still extremely rare. For a person with uncontrolled diabetes, the risk of heart attack, stroke, or kidney failure is far higher. So the FDA didn’t pull the drug. They updated the label. Doctors now screen patients for risk factors - like diabetes control, obesity, or prior genital infections - before prescribing. The result? The infection is still rare. But doctors are now aware. Patients are informed. Deaths dropped. That’s risk-benefit assessment working as intended.Final Thought: It’s a Judgment, Not a Math Problem
Dr. Janet Woodcock, former head of the FDA’s drug center, said it best: "Risk-benefit is not a calculation. It’s a judgment." It’s not about numbers alone. It’s about your life. Your health. Your priorities. A 1 in 10,000 risk might be unacceptable if you’re young and healthy. It might be worth it if you’re 70 with heart failure and no other options. The FDA gives you the data. Your doctor helps you weigh it. You make the decision - with full information, not fear.Should I stop taking my medication if I see an FDA safety alert?
No. FDA safety alerts are not instructions to stop medication. They are signals that more data is being reviewed. Stopping a prescribed drug without medical advice can be dangerous - especially for conditions like high blood pressure, epilepsy, or depression. Always talk to your doctor before making any changes.
What’s the difference between a "potential signal" and a "confirmed risk"?
A "potential signal" means the FDA has noticed a pattern in reports that might suggest a new risk, but there isn’t enough evidence yet to prove the drug causes it. A "confirmed risk" means the FDA has reviewed enough data - including studies and real-world use - to conclude the drug likely causes the problem. Only confirmed risks lead to official label changes or new safety requirements.
Why don’t FDA alerts always include numbers like "1 in 1,000"?
Many older alerts lack quantitative risk estimates because the data isn’t fully analyzed yet. The FDA is working to fix this. Starting in 2025, all new communications will include standardized risk numbers. Until then, ask your doctor: "What’s the actual risk?" and "How does it compare to the benefit?"
Can I trust FDA alerts if they sometimes turn out to be wrong?
Yes - because the system is designed to catch problems early, even if some signals turn out to be false alarms. It’s better to alert the public to a possible risk and later clarify than to miss a real danger. The FDA has improved transparency over time, and now clearly labels alerts as "potential" or "confirmed."
How do I know if my drug is affected by a recent FDA alert?
Check the FDA’s Drug Safety Communications page (fda.gov/drugs/drug-safety-and-availability) and search for your drug’s name. You can also check the "Warnings and Precautions" section of your medication’s prescribing information, which is updated when the FDA requires labeling changes. Your pharmacist can also help you find this information.

Harsh Khandelwal
December 23, 2025 AT 17:37So let me get this straight - the FDA says ‘potential signal’ and we’re supposed to chill? Bro, they’re the same people who let OxyContin ride shotgun to the apocalypse while telling docs it was ‘low risk.’ Now they wanna be the hero? I’m not trusting a system that still hasn’t admitted they missed 3,000+ deaths from Vioxx because ‘the data wasn’t conclusive enough.’
They don’t want us to panic? Then stop releasing alerts like they’re TikTok notifications. ‘Drug X may cause spontaneous nosebleeds in people who sneeze on Tuesdays.’ Come on. I’d rather just Google my symptoms and pray.
Spencer Garcia
December 24, 2025 AT 02:58Important context here: FDA alerts are early warnings, not verdicts. If you’re on a life-saving med, don’t stop cold turkey. Talk to your doc. Most ‘risks’ are statistical noise - like worrying about being struck by lightning while crossing the street because someone else got hit.
The real takeaway? Stay informed, don’t panic, and use the five questions in the post. That’s how you make smart choices - not fear-based ones.
Abby Polhill
December 26, 2025 AT 00:04As someone who works in pharmacovigilance, I’ll say this: the FAERS database is a goldmine - but it’s also a dumpster fire of confounders. A report of ‘headache after taking metformin’? Could be stress, dehydration, caffeine withdrawal, or just Tuesday. The FDA’s job is to filter signal from the noise - and honestly? They’re doing better than most realize.
What’s missing? Absolute risk quantification. But 2025’s standardized format is gonna fix that. Until then, ask your prescriber: ‘What’s the NNT vs. NNH?’ If they stare blankly, you’ve got your answer.
Bret Freeman
December 27, 2025 AT 07:43Let’s be real - this whole system is a corporate shill fest. Big Pharma pays the FDA to look the other way. The ‘potential signal’ language? That’s a legal loophole so they can keep selling drugs while pretending they’re ‘being cautious.’
I saw a guy on YouTube say his cousin died from ‘Drug Y’ after the FDA alert came out - and guess what? The company didn’t even update the label for 18 months. That’s not safety. That’s profit protection dressed up as science.
Don’t believe the fairy tale. The FDA doesn’t protect you. Your doctor, if they’re actually listening, might.
Lindsey Kidd
December 28, 2025 AT 01:51Y’all need to breathe 😌
I’ve been on a med that had an FDA alert - turned out the risk was 0.0004%. My doctor said, ‘You’re 32, active, no other risk factors - this isn’t your problem.’ I kept taking it. Still here. Still healthy.
Don’t let headlines hijack your peace. Talk to your provider. They know your story - not just the data. 💪❤️
Rachel Cericola
December 28, 2025 AT 16:42Look, I get why people panic - medication alerts feel personal. But the real danger isn’t the drug. It’s the misinformation cycle. People read ‘possible link’ and immediately assume ‘guilty until proven innocent.’ That’s not how science works.
Let me break it down: if you’re on a drug for bipolar disorder, and the FDA says ‘possible increased risk of tremors,’ you don’t quit cold turkey - you call your psychiatrist. Tremors are manageable. Relapse isn’t.
The FDA’s system isn’t perfect, but it’s the only one that’s transparent enough for you to actually investigate. You want to know if a risk is real? Go to the source. Read the full communication. Look at the numbers. Don’t rely on Reddit, Twitter, or your aunt who read a blog post about ‘toxic pharmaceuticals.’
And if your doctor dismisses your concern? Get a second opinion. But don’t self-prescribe fear. That’s the real poison.
This isn’t about blind trust. It’s about informed action. And that requires patience, critical thinking, and a willingness to sit with uncertainty - which, let’s be honest, most of us suck at.
So next time you see an alert, take a breath. Pull up the FDA page. Read the fine print. Ask your doctor the five questions in the post. Then decide. Not react. Decide.
Katie Taylor
December 29, 2025 AT 06:44STOP. RIGHT. NOW. If you’re thinking of quitting your med because of an FDA alert, you’re literally risking your life. I’ve seen people go into diabetic ketoacidosis because they panicked over a ‘possible’ risk that turned out to be less likely than winning the lottery while getting struck by lightning.
You don’t get to play roulette with your health because some algorithm screamed ‘DANGER’ on the news. Talk to your doctor. That’s it. That’s the whole fucking point.
Payson Mattes
December 31, 2025 AT 06:15Hey, I just looked up my med - turns out the FDA alert was from 2021, and the label hasn’t changed. But here’s the thing - did you know the FDA’s database allows you to search by patient age, gender, and comorbidities? I did. And guess what? My risk is actually lower than average because I’m healthy and under 40.
Also, I reported my mild rash last year. They sent me a thank-you email. That’s how you help. Not by quitting your med - by contributing data. You’re not just a patient. You’re a scientist now. 🧪
Isaac Bonillo Alcaina
January 1, 2026 AT 15:09The post is technically accurate, but it exhibits a dangerous level of institutional deference. The FDA is not a neutral arbiter - it is a regulatory body embedded within a profit-driven pharmaceutical ecosystem. The ‘potential signal’ language is deliberately ambiguous to avoid litigation and maintain stock prices.
Furthermore, the assertion that ‘the system is getting better’ is unsupported by evidence. The 2024 guidance was issued after public outcry, not internal reform. And the ‘standardized risk formats’? They’ll be optional until 2027, and even then, they’ll be buried in PDF appendices.
This isn’t about trust. It’s about power. And until patients demand transparency as a right - not a privilege - we’re all just data points in a corporate risk model.
Joseph Manuel
January 2, 2026 AT 07:23The post misrepresents the nature of FDA safety communications by implying they are primarily patient-facing educational tools. In reality, they are risk management instruments designed for clinicians and regulatory stakeholders. The language is intentionally conservative to avoid liability, not to confuse patients.
Moreover, the claim that ‘the system is getting better’ is statistically unfounded. The volume of adverse event reports has increased 400% since 2010, but the rate of confirmed risk determinations has remained flat - suggesting increased noise, not improved signal detection.
Patients should not be expected to interpret FAERS data. That is the role of the prescriber. The onus should not be on the layperson to navigate statistical ambiguity - it should be on the regulatory body to communicate with clarity and urgency when the risk-benefit calculus shifts meaningfully.