Immunocompromised Patients and Medication Reactions: What You Need to Know
Immunosuppression Risk Calculator
Personalized Risk Assessment
Calculate your individual infection risk based on the immunosuppressant medication you're taking, your dosage, and treatment duration. This tool uses clinical data from the article to provide personalized risk assessment.
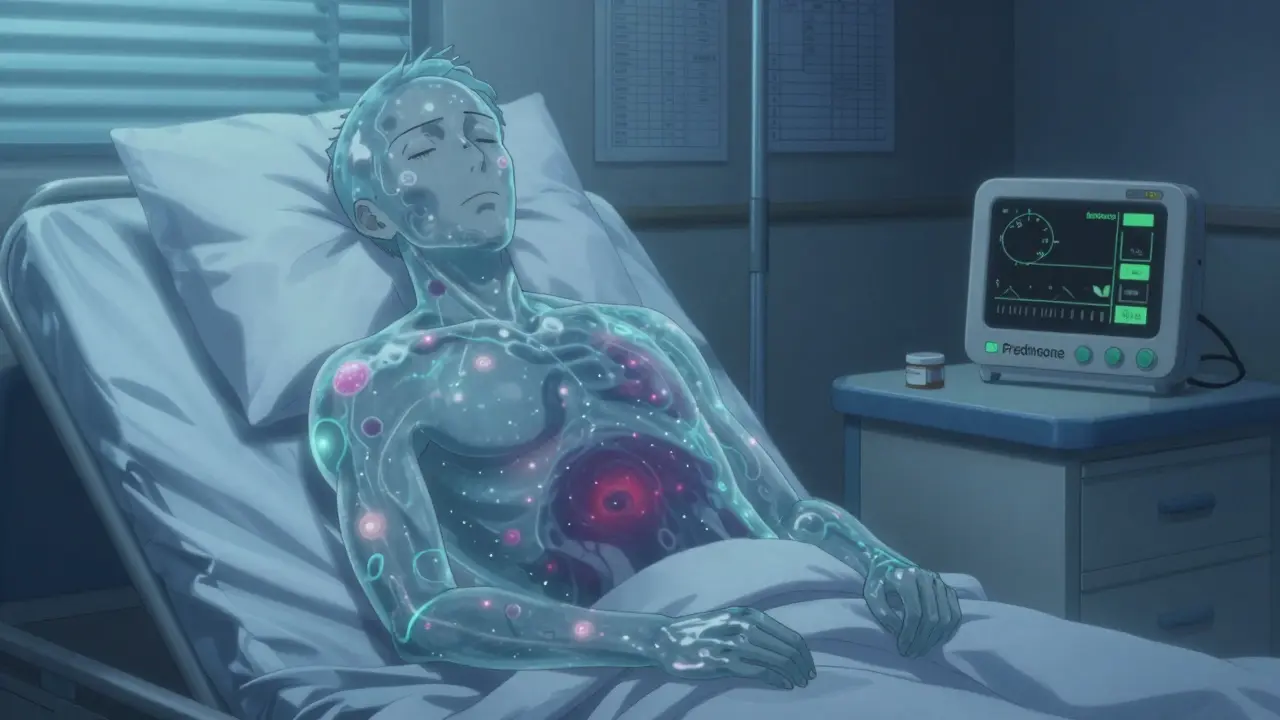
When your immune system is weakened-whether from disease, transplant, or long-term medication-you don't just get sick more often. You get sicker. And sometimes, the signs of illness don't look like what you'd expect. For immunocompromised patients, even a common cold can turn dangerous. A simple fever might not show up. An infection might creep in without redness or swelling. And the very drugs meant to help can quietly increase your risk of life-threatening complications.
What Does It Mean to Be Immunocompromised?
Being immunocompromised means your body's defense system isn't working the way it should. It doesn't mean you're weak. It means your immune cells-T cells, B cells, macrophages-are either damaged, suppressed, or outnumbered. This can happen for many reasons: organ transplants, chemotherapy, HIV, lupus, rheumatoid arthritis, or long-term use of drugs like prednisone or methotrexate. The Cleveland Clinic says it simply: "You might get sick more often or more severely than others."
But here’s the twist: not all immunosuppression is the same. A person on low-dose prednisone for a few weeks after a flare-up has a very different risk profile than someone on a biologic for ten years. The type of medication, the dose, and how long you’ve been on it all matter. And that’s why blanket advice doesn’t work.
The Big Risk: Infections That Don’t Look Like Infections
Most people know to watch for fever, chills, or a sore throat. But for someone on immunosuppressants, those signs can vanish. Corticosteroids like prednisone and dexamethasone blunt your body’s natural alarm system. A 2005 study cited by the PMC journal found these drugs can hide the classic symptoms of infection. You might not run a fever. Your white blood cell count might stay normal. But the infection is still there-growing, spreading, silently damaging.
That’s why patients on long-term steroids often don’t realize they’re sick until it’s too late. One woman in Dublin, on methotrexate for psoriatic arthritis, thought she had the flu after a weekend trip. She didn’t feel feverish. No cough. Just tired. By the time she went to the hospital, she had sepsis from an undiagnosed urinary tract infection. Her immune system had been too quiet to sound the alarm.
Common infections become dangerous. Pneumocystis pneumonia, cytomegalovirus (CMV), herpes zoster (shingles), and even tuberculosis can strike without warning. And some infections aren’t even from germs you catch from others. The JC virus, which lives quietly in most people’s brains, can reactivate and cause progressive multifocal leukoencephalopathy (PML)-a rare but deadly brain infection linked to certain biologics.
How Different Drugs Carry Different Risks
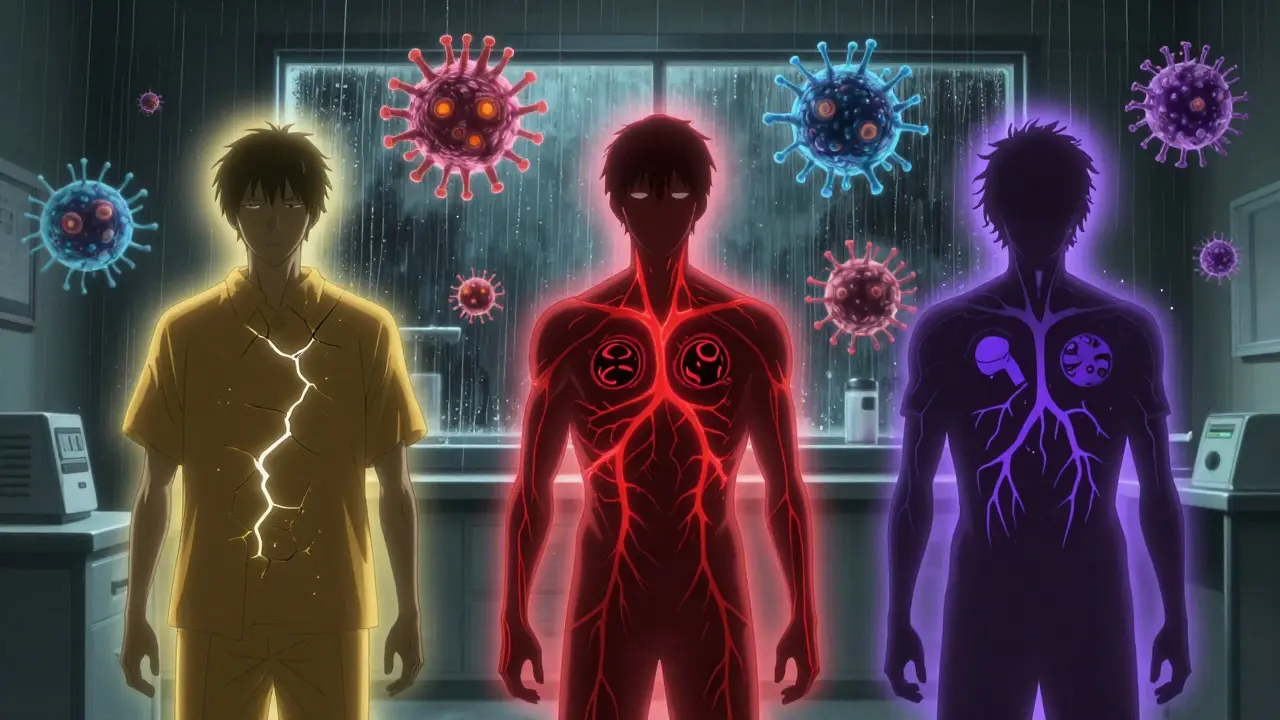
Not all immunosuppressants are created equal. Each class works differently-and each has its own danger zone.
- Corticosteroids (prednisone, methylprednisolone): Risk jumps sharply above 20mg/day of prednisone equivalent. Even short courses longer than two weeks can raise infection risk. A 2012 meta-analysis of over 4,000 patients found steroid users had a 12.7% chance of infection-compared to 8% in those not taking them. That’s a 60% higher risk.
- Methotrexate: Used for rheumatoid arthritis, psoriasis, and Crohn’s. It’s effective for most, but about half of users quit within a year because of side effects: nausea, fatigue, mouth sores. Liver toxicity and low blood counts are real concerns. Monthly blood tests are standard for safety.
- Azathioprine: Reduces T and B cells. Its biggest danger? Leukopenia (low white blood cells). When that happens, bacterial infections and viruses like hepatitis B or CMV can flare. PML risk is low but real.
- Biologics (TNF inhibitors, IL-6 blockers): These are powerful. They target specific parts of the immune system, but that precision comes at a cost. Research from the Arthritis Foundation says they’re "significantly more likely to lead to infections" than older drugs. Many Reddit users in autoimmune communities report hospitalizations for shingles or pneumonia after starting adalimumab or infliximab.
- Calcineurin inhibitors (cyclosporine, tacrolimus): Common after transplants. They carry high risks for viral infections: EBV, hepatitis C, and polyomavirus. One transplant patient described tacrolimus as "life-changing"-but only after learning to check for fever daily and avoid crowded places during flu season.
- Chemotherapy agents (cyclophosphamide, paclitaxel): These are broad-spectrum immune killers. They wipe out dividing cells-including immune cells. Infection risk here is among the highest of all.
And combining drugs? That’s where things get risky. Using steroids with methotrexate, or biologics with azathioprine, doesn’t just add risks-it multiplies them. The PMC article on infections in immunocompromised hosts says the combination creates a "synergistic effect," meaning the whole is worse than the sum of its parts.
What About Vaccines? Can You Still Get Them?
Yes-but not all vaccines are safe. Live vaccines (like MMR, varicella, nasal flu spray) are generally off-limits. They contain weakened viruses that could spread in a suppressed immune system. Instead, you need inactivated versions: the flu shot, Tdap, pneumococcal, and hepatitis B vaccines.
Timing matters. Ideally, you get vaccinated before starting immunosuppressants. Once you’re on them, your immune system may not respond well. Studies show antibody levels after vaccination are often lower. That doesn’t mean it’s useless-it just means you need to be extra careful. The CDC recommends extra doses of COVID-19 vaccines for immunocompromised people, and many now get boosters every 6 months.
And here’s something surprising: research from Johns Hopkins in 2021 found that immunosuppressed patients didn’t have worse outcomes from COVID-19 than the general population. That overturned years of assumptions. It turns out, in some cases, suppressing immune overreaction (like cytokine storms) might actually help. But this doesn’t mean you should stop taking precautions. It just means personalized care matters more than ever.
Prevention Isn’t Optional-It’s Daily
There’s no magic pill to protect you. Prevention is a habit. Here’s what actually works:
- Wash your hands for at least 20 seconds-don’t skip your nails or between your fingers. Alcohol-based sanitizer works when soap isn’t available.
- Wear a mask in crowded places, especially during flu season or outbreaks. N95 or KN95 masks are better than cloth.
- Practice wound care. Even a small cut can become infected. Clean it, cover it, and watch for redness or swelling.
- Avoid high-risk environments. Stay away from construction sites, bird droppings, soil gardens, and undercooked meat. Fungi and bacteria thrive there.
- Watch for vector-borne diseases. The CDC warns immunocompromised people are at higher risk from tick- and mosquito-borne illnesses like Lyme disease or West Nile virus. Use repellent, wear long sleeves.
- Know your body. If you feel off-tired, achy, dizzy, confused-don’t wait. Call your doctor. Don’t assume it’s just a side effect.
One patient in an online forum said it best: "I used to think I was fine if I didn’t have a fever. Now I know: if I feel like I’ve been hit by a truck, I’m already behind."
Monitoring: Blood Tests, Not Just Symptoms
Your doctor doesn’t rely on how you feel. They rely on numbers.
- Complete Blood Count (CBC): Checks for low white cells, anemia, or platelet drops. For methotrexate, this is done monthly at first.
- Liver and kidney function tests: Methotrexate and azathioprine can stress these organs. Abnormal results mean a dose change or switch is needed.
- Viral screenings: Before starting biologics or calcineurin inhibitors, you’re tested for hepatitis B, hepatitis C, and TB. Reactivation is real.
Some patients skip these tests because they feel fine. That’s dangerous. Infections can grow quietly. A drop in lymphocytes doesn’t come with symptoms. But it can mean the difference between a quick antibiotic and a hospital stay.

When the Benefits Outweigh the Risks
Let’s be honest: immunosuppressants save lives. They prevent organ rejection. They stop autoimmune diseases from destroying joints, skin, or organs. A woman with lupus might not walk without steroids. A transplant patient might not survive without tacrolimus.
The goal isn’t to avoid these drugs-it’s to use them wisely. That means:
- Starting with the lowest effective dose
- Using short courses when possible (like prednisone for a flare)
- Choosing targeted therapies over broad suppression
- Monitoring closely and adjusting fast
And yes-some people do better than others. Genetics, age, diet, and other health conditions all play a role. One person on methotrexate might feel great for years. Another might need to switch after six months. That’s why shared decision-making matters. You need to know your personal risk-not just the textbook numbers.
The Future: Personalized Immunosuppression
The next big leap isn’t just better drugs-it’s smarter dosing. Researchers are exploring pharmacogenomics: using your genes to predict how you’ll respond to a drug. Some people metabolize azathioprine too fast. Others too slow. A simple blood test could tell you if you’re at risk for toxicity before you even start.
JAK inhibitors are already offering more targeted suppression than older drugs. And new biomarkers are being tested to predict infection risk before it happens. Imagine a blood test that says: "Your immune system is at 70% capacity this week-avoid travel." That’s not science fiction. It’s coming.
But until then, the rules are simple: stay vigilant, stay informed, and don’t ignore the quiet signs. Your immune system might not scream. But it’s still speaking.
Can immunosuppressants cause long-term damage?
Yes, some immunosuppressants can cause long-term issues. Methotrexate may lead to liver scarring over time, especially with alcohol use. Azathioprine and cyclophosphamide carry a small but real risk of certain cancers, like lymphoma. Long-term corticosteroids can cause osteoporosis, diabetes, and cataracts. That’s why regular monitoring and dose adjustments are critical. The goal is to use the minimum effective dose for the shortest time possible.
Is it safe to be around sick people if I’m immunocompromised?
It’s risky. Even mild illnesses like the common cold can become serious. Avoid close contact with anyone who’s sick. If a family member has a cold, ask them to wear a mask around you, wash hands often, and avoid sharing items. If you’re exposed and start feeling unwell, contact your doctor immediately-even if you don’t have a fever.
Do I need to stop my medication before surgery?
Sometimes. It depends on the drug and the surgery. Corticosteroids may need to be temporarily increased before surgery to prevent adrenal crisis. Biologics are often paused 1-2 weeks before and after surgery to reduce infection risk. Never stop medication without talking to your doctor. A sudden stop can trigger a disease flare or even organ rejection.
Can I travel if I’m immunocompromised?
Yes-but with caution. Avoid areas with high infection risk (like regions with poor sanitation or outbreaks). Get travel vaccines approved for your condition. Carry a letter from your doctor listing your medications. Bring extra doses in case of delays. Avoid cruises, large crowds, and poorly ventilated spaces. Always have access to medical care while traveling.
Why do some immunocompromised patients do better than others?
It’s not just the drug-it’s the person. Age, other health conditions (like diabetes or lung disease), nutrition, sleep, and stress levels all affect immune resilience. Someone with a healthy diet, regular sleep, and low stress may handle immunosuppression better than someone with chronic inflammation or poor nutrition. Genetics also play a role in how your body processes medications. Personalized care makes all the difference.
What Comes Next?
If you’re immunocompromised, your care team should be your partner-not just your prescriber. Ask questions. Track your symptoms. Know your numbers. Don’t let fear stop you from living-but don’t let complacency put you at risk.
The future of immunosuppression isn’t about shutting down the immune system. It’s about tuning it. Precision. Monitoring. Prevention. And above all-listening.

Tasha Lake
February 7, 2026 AT 17:36Just read through this and had to pause-this is some next-level stuff. The part about corticosteroids masking fever? That’s wild. I’ve got a friend on prednisone for lupus, and she swears she’s fine until she’s not. No fever, no chills, just… exhausted. Then boom, sepsis. It’s terrifying how silently these infections creep in. I’m starting to think we need a wearable that tracks lymphocyte trends in real time. Like a Fitbit for your immune system.