Irritable Bowel Syndrome: How the Gut-Brain Axis Causes Symptoms and What Actually Helps
For millions of people, stomach pain, bloating, and sudden changes in bowel habits aren’t just inconvenient-they’re life-limiting. If you’ve been told it’s "just stress" or "all in your head," you’re not alone. But here’s the truth: irritable bowel syndrome isn’t a psychological disorder. It’s a real, measurable breakdown in communication between your gut and your brain. And understanding that connection is the key to real relief.
What IBS Really Is (And What It Isn’t)
Irritable bowel syndrome, or IBS, affects between 5% and 10% of people worldwide. It’s not an infection. It’s not cancer. It’s not something you can see on a colonoscopy. That’s why so many people go years without a proper diagnosis. The Rome IV criteria, used by doctors since 2016, define IBS by three things: recurrent abdominal pain at least one day a week over the last three months, plus at least two of these: pain linked to bowel movements, changes in how often you go, or changes in stool appearance. But here’s what most doctors don’t tell you: 76% of people with IBS also feel persistent discomfort-not full pain-just a constant, nagging pressure. And 60-70% also struggle with anxiety or depression. Not because they’re weak. Because their nervous system is stuck in overdrive.The Gut-Brain Axis: Your Body’s Hidden Wiring
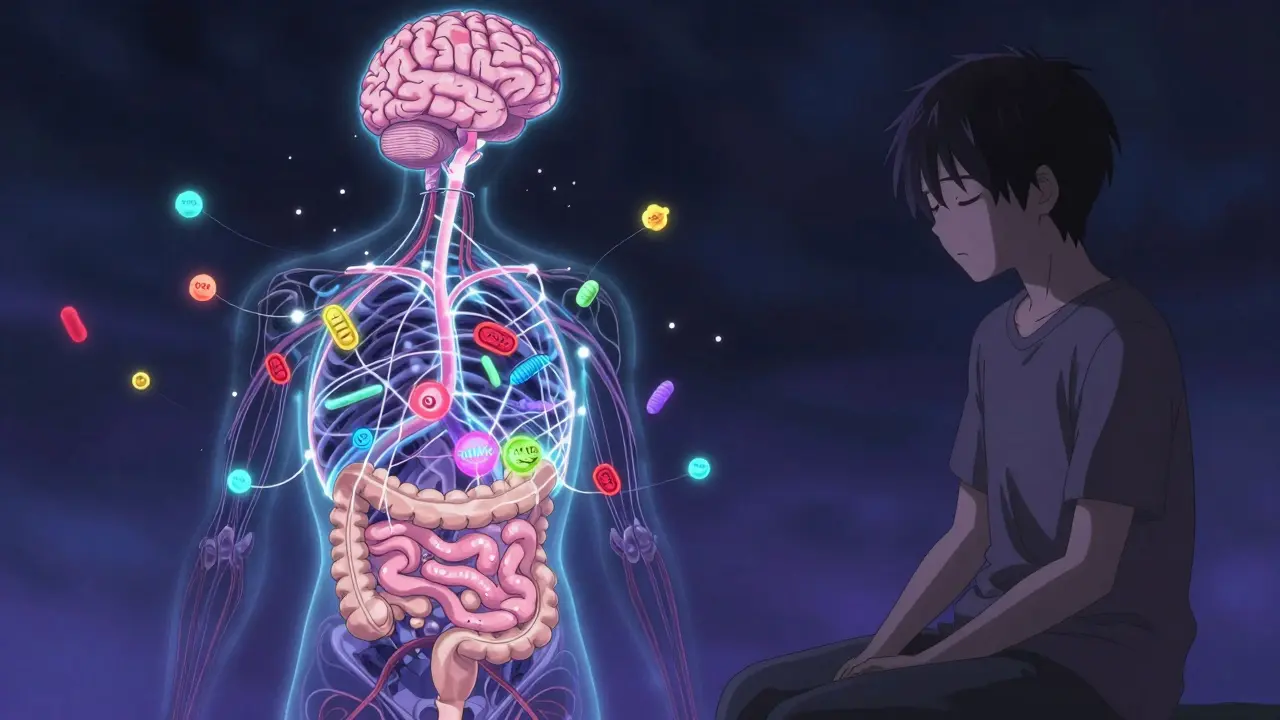
Your gut has its own nervous system-called the enteric nervous system-and it’s wired directly to your brain through the vagus nerve. This two-way street is called the gut-brain axis. It controls digestion, appetite, and even how you feel pain. In IBS, this system gets tangled. Signals get mixed up. Your brain starts interpreting normal gut movements as painful. Your gut starts reacting to stress like it’s under attack. Brain scans show clear differences in people with IBS. Those with diarrhea-predominant IBS (IBS-D) have thicker brain areas linked to sensing bodily sensations. Those with constipation-predominant IBS (IBS-C) show thinner areas in regions that help regulate emotion and pain. These aren’t random changes. They’re physical adaptations to chronic gut distress. Serotonin plays a huge role. Ninety-five percent of your body’s serotonin is made in your gut-not your brain. In IBS-D, levels of serotonin in the gut lining are nearly 60% higher than in healthy people. That speeds up movement, leading to diarrhea. In IBS-C, serotonin is too low, slowing everything down. This isn’t about mood. It’s about nerve signaling. Your gut microbes-bacteria, fungi, viruses-also talk to your brain. Studies show people with IBS have different ratios of Firmicutes to Bacteroidetes bacteria. These microbes produce chemicals that influence nerve activity, inflammation, and even your stress response. When they’re out of balance, your gut-brain axis gets noisy.Why Traditional Treatments Often Fail
Antispasmodics, laxatives, and anti-diarrheal meds like loperamide are still commonly prescribed. But they only mask symptoms. They don’t fix the broken signal. A 2022 survey of over 45,000 IBS patients found that 63% had side effects from these drugs. Nearly half stopped taking them within three months because the relief didn’t last-or the side effects were worse than the symptoms. The real problem? Most treatments treat the gut as if it’s isolated. But if your brain is misreading signals from your gut, no pill will fix that. You need to reset the communication line.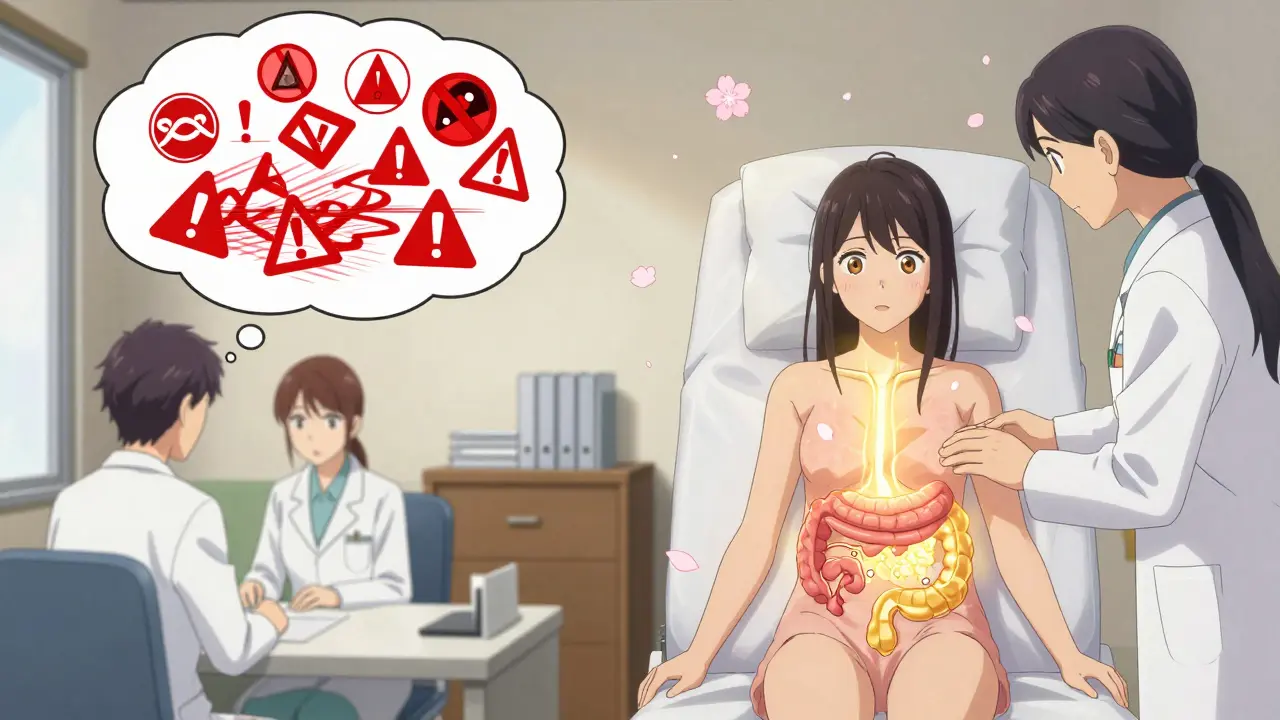
What Actually Works: Science-Backed Relief
1. The Low-FODMAP DietThis isn’t just another fad. In clinical trials, 50-76% of people with IBS saw major symptom improvement on a low-FODMAP diet. FODMAPs are short-chain carbs found in onions, garlic, wheat, dairy, and artificial sweeteners. They ferment quickly in the gut, pulling in water and producing gas. That distends the intestine-and if your nerves are hypersensitive, that feels like severe pain. The diet works in three phases: elimination, reintroduction, and personalization. It’s hard. The first phase lasts 4-6 weeks. But for many, it’s the most effective tool they’ve ever tried. One Reddit user wrote: "After 5 years of doctors telling me it was stress, low-FODMAP gave me back my life." 2. Gut-Directed Hypnotherapy
This isn’t stage hypnosis. It’s a structured, evidence-based therapy where you learn to calm your nervous system using guided imagery. Studies show 70-80% of people respond to it. That’s better than most medications. The effects last-at least six months after treatment ends. It works by teaching your brain to stop overreacting to normal gut activity. A 2021 trial found it doubled the response rate compared to standard care. The catch? It’s expensive. A full course costs $1,200-$2,500. And trained therapists are rare. In rural areas, you might find one provider for every 500,000 people. 3. Probiotics That Actually Work
Not all probiotics help. Most don’t. But one strain-Bifidobacterium infantis 35624-has been tested in multiple trials. Taken daily at 1 billion CFUs, it improved global IBS symptoms in 30-40% of people. That’s double the placebo effect. It works by reducing inflammation and calming nerve activity in the gut lining. Other strains? Not proven. 4. New Drugs Targeting the Gut-Brain Axis
For IBS-D, alosetron (a 5-HT3 blocker) helps 50-60% of women, but it carries a risk of severe constipation and colon damage-so it’s only for severe cases. For IBS-C, prucalopride (a 5-HT4 agonist) improves bowel movement frequency in 45-55% of users. And a new drug, etrasimod, showed 52% symptom improvement in a 2023 phase III trial-nearly twice the placebo effect. These aren’t magic bullets, but they’re the first drugs designed to fix the gut-brain signal, not just the symptom. 5. Vagus Nerve Stimulation
A small but growing number of people are using non-invasive devices that stimulate the vagus nerve through the skin (tVNS). Early studies show 45-55% reduction in abdominal pain. It’s not FDA-approved for IBS yet, but trials are underway. It’s cheap, safe, and you can use it at home.
What’s Next: Personalized IBS Care
In 2023, a new blood and stool test called VisceralSense™ launched. It measures 12 microbial metabolites and serotonin ratios to predict which treatment will work for you-with 85% accuracy. This isn’t science fiction. It’s real. And it’s the future. The NIH just launched a $15 million project to build personalized treatment algorithms based on your unique gut-brain profile. Within five years, your IBS treatment may be chosen by a computer analyzing your microbiome, brain activity, and genetic markers.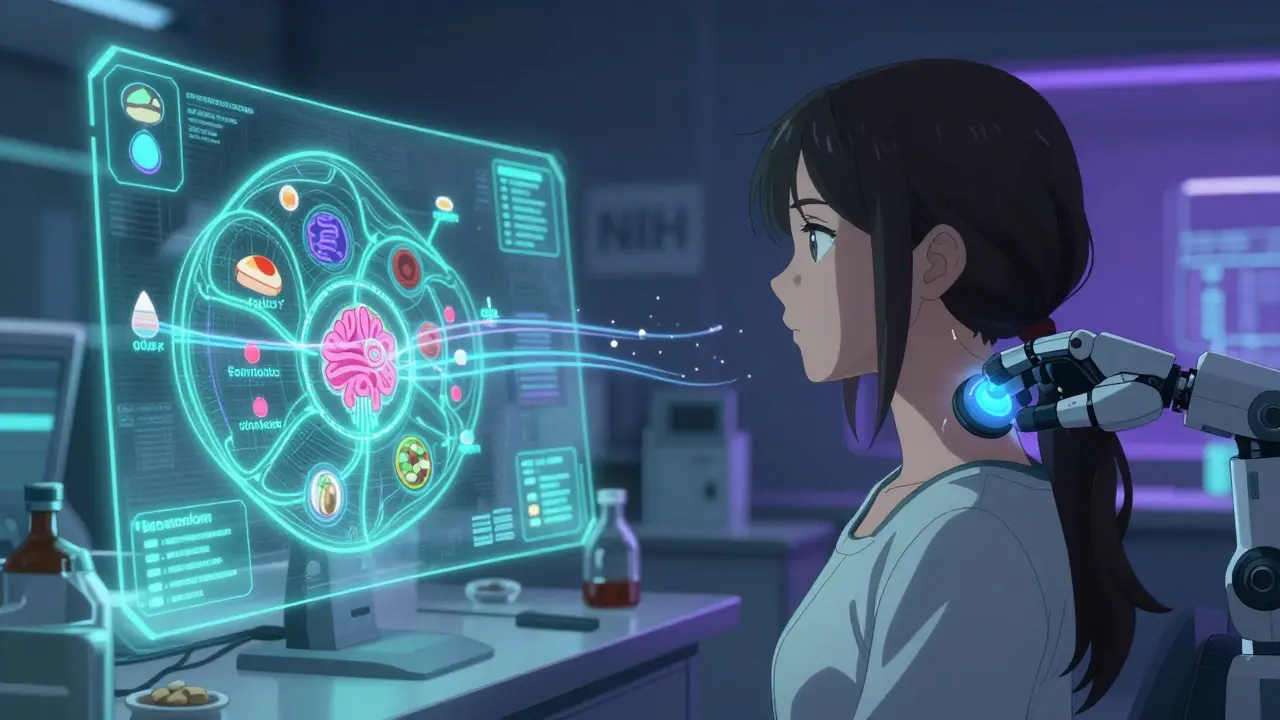
Getting Started: A Simple Plan
You don’t need to do everything at once. Start here:- Get educated. Read about the gut-brain axis. Understanding it reduces fear-and improves outcomes. People who understand the science stick with treatment 30% longer.
- Try the low-FODMAP diet with a dietitian. Don’t guess. Use a reliable app or guide. Track your symptoms daily.
- Look for a certified gut-directed hypnotherapist. Search the American Society of Clinical Hypnosis directory.
- If symptoms persist, ask your doctor about serotonin-targeted meds or tVNS devices.

Sarah Triphahn
January 14, 2026 AT 15:16So let me get this straight - we’re now treating IBS like it’s a glitch in your phone’s software? Fix the signal, reset the app, reboot your gut. Meanwhile, people are still dying from colon cancer because doctors won’t order a real scan. This is just pharmaceutical marketing with a side of yoga.
Low-FODMAP? I tried it. Lost 15 pounds. Got called ‘anorexic’ by my mom. Still had pain. Now I just eat steak and cry in peace.
Vicky Zhang
January 16, 2026 AT 09:16OH MY GOSH I CRIED READING THIS. I’ve been suffering for 12 years and every doctor said ‘it’s anxiety’ until I found gut-directed hypnotherapy. It didn’t fix everything but it gave me back my weekends. I used to cancel plans because I was scared I’d have an accident in public. Now I go to concerts. I travel. I eat garlic again (carefully). This isn’t just science - it’s liberation. If you’re reading this and still feeling alone - you’re not. We’re here. We’ve been there. You deserve relief. You’re not broken. Your body is just screaming and nobody was listening. But now? Now we’re finally hearing it.
I’m so proud of you for even clicking on this post. That’s the first step. I believe in you.
Send me a DM if you need help finding a therapist. I’ll send you my favorite resources. No judgment. Ever.
Allison Deming
January 16, 2026 AT 20:38It is deeply concerning that the medical establishment continues to treat gastrointestinal distress as a purely somatic condition, while simultaneously dismissing the profound psychosomatic interplay that has been empirically documented for decades. The notion that serotonin regulation in the enteric nervous system constitutes a ‘cure’ is not only reductionist - it is dangerously neoliberal, outsourcing biological complexity to pharmacological bandaids while ignoring systemic contributors: food deserts, chronic stress from economic precarity, and the erosion of communal care structures that once supported digestive health.
Probiotics? Hypnotherapy? These are bandages on a severed artery. Until we address the sociopolitical architecture of illness - the wage slavery that keeps people eating processed foods, the lack of paid sick leave, the stigma around mental health - we are merely rearranging deck chairs on the Titanic. Your ‘personalized algorithm’ is a capitalist fantasy. Real healing requires collective action, not a $2,500 app subscription.
Susie Deer
January 16, 2026 AT 23:45Low FODMAP is a scam. America is weak. Eat real food. No apps. No therapy. Just stop eating carbs and gluten. My grandpa ate lard and cornbread his whole life and never had a stomach problem. This is all modern nonsense. Stop coddling your gut. Your body is fine. You’re just soft.
Also probiotics are for hippies. Real men take antibiotics and shut up.
TooAfraid ToSay
January 18, 2026 AT 23:03Hold up. You say 95% of serotonin is in the gut? Then why does Prozac work for IBS? If your brain is the problem, why blame the bacteria? And why are all the ‘science-backed’ treatments from the US? What about Nigeria? We eat pounded yam with pepper soup every day and no one’s doing hypnotherapy. We just pray and eat more pepper. Maybe your gut is broken because you think too much. Maybe the answer isn’t more tech - it’s less thinking.
Also I read this article on my phone while eating fried plantain. My stomach is fine. You’re all overthinking. Maybe IBS is just a Western disease. Like TikTok anxiety.
Dylan Livingston
January 20, 2026 AT 22:46Oh how darling. Another feel-good manifesto disguised as medical insight. The low-FODMAP diet? A trendy, overpriced elimination protocol that turns people into food neurotics who measure their anxiety in grams of onion powder. And hypnotherapy - because nothing says ‘evidence-based’ like whispering about calm seas while someone imagines their colon is a spa. How very 2023. Meanwhile, real science is in the lab, developing targeted biologics, not in Reddit threads where people trade trauma like trading cards. And don’t get me started on the ‘vagus nerve stimulation’ gadgets - next you’ll be selling crystals that ‘align your gut chi.’
The only thing ‘personalized’ here is the marketing. You’re selling hope to the desperate. And that’s not healing - that’s exploitation dressed in lab coats.
Andrew Freeman
January 21, 2026 AT 13:04low fodmap is a joke i tried it for 3 weeks and i was hungrier than ever. why do we need an app to tell us not to eat onions? my grandma just ate what she had and lived to 92. also probiotics? my dog takes them and still poops on the rug. stop overcomplicating your body. eat less junk. move more. stop staring at screens. your gut is not a wifi router.
also i tried hypnotherapy once. the lady said ‘imagine your intestines are happy dolphins’ and i fell asleep. woke up with a headache. no thanks.
says haze
January 22, 2026 AT 19:06The entire discourse around IBS remains trapped in a reductive biopsychosocial model that fetishizes individual agency while erasing the epistemic violence of diagnostic neglect. The fact that 76% of patients report persistent discomfort - not pain, but discomfort - speaks not to neural hypersensitivity alone, but to the institutional failure to recognize visceral suffering as legitimate unless it manifests in visible pathology.
The low-FODMAP diet, while statistically effective, is a symptom management strategy that pathologizes dietary diversity. It transforms nutrition into a minefield. The hypnotherapy industry, meanwhile, commodifies neuroplasticity into a luxury service accessible only to the insured and the educated. And the new pharmacological interventions? They’re not cures - they’re temporal palliatives wrapped in the language of innovation.
The real breakthrough isn’t in serotonin ratios or microbial metabolites. It’s in the collective refusal to accept that chronic illness must be managed, not understood. We must shift from treating bodies to listening to them - not through apps, not through therapists, but through structural compassion. The gut-brain axis isn’t broken. The system is.