Liver Transplantation: Eligibility, Surgery, and Immunosuppression Explained
When your liver fails, there’s no backup. Unlike other organs, the liver doesn’t just slow down-it shuts down fast. For people with end-stage liver disease, a transplant isn’t just an option. It’s the only thing that can bring them back to life. In 2023, over 8,000 people in the U.S. received a new liver. Most of them survived at least one year. But getting there isn’t simple. It’s a long, strict, and highly personalized process that starts long before the operating room.
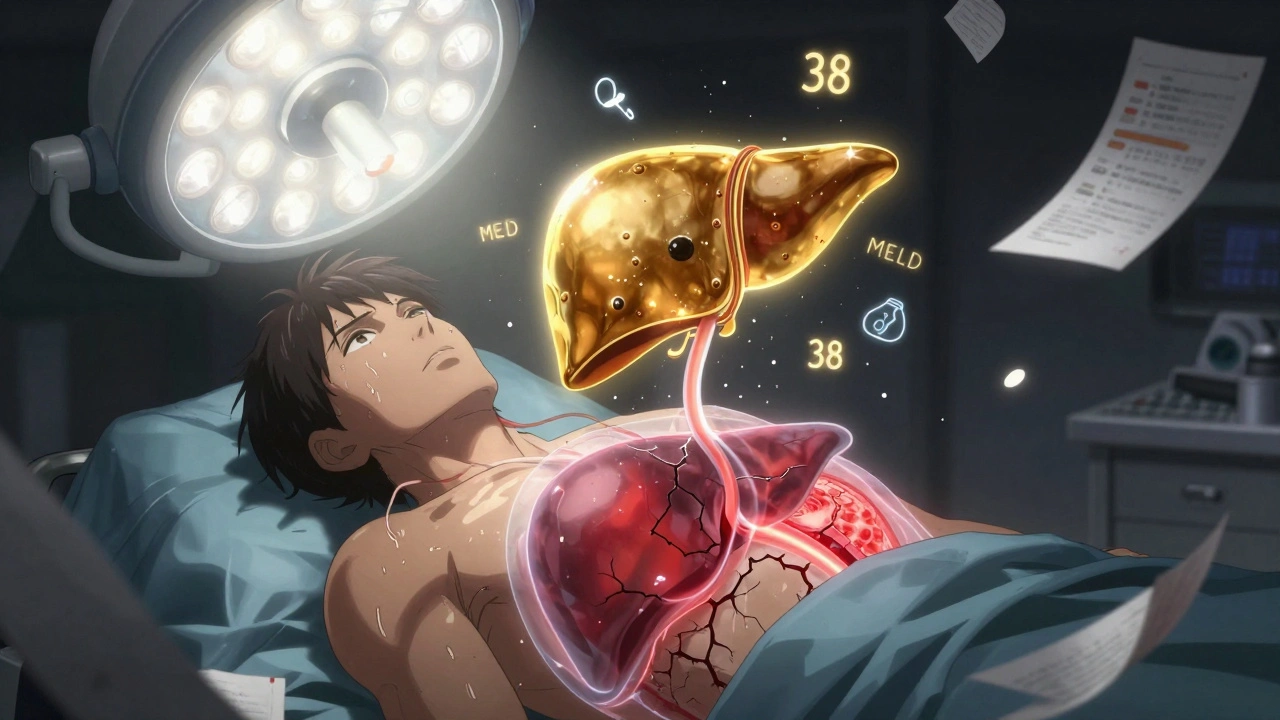
Who Gets a Liver Transplant?
Not everyone with liver disease qualifies. The decision isn’t based on how sick you feel. It’s based on numbers-cold, hard, medical data. The MELD score is the gatekeeper. It uses blood tests for bilirubin, creatinine, and INR to predict your chance of dying in the next three months. A score of 6 means you’re relatively stable. A score of 40 means you’re in critical condition. The higher your score, the higher your priority on the waiting list.But numbers aren’t everything. If you’re still drinking alcohol or using drugs, you’re not eligible. Most centers require at least six months of sobriety before listing. That rule isn’t the same everywhere. Some centers are starting to accept three months, especially if you’re in a structured recovery program. Others still stick to six. It depends on the team, the region, and your individual case.
People with liver cancer can also qualify-but only if their tumors are small and contained. The Milan criteria are strict: one tumor under 5 cm, or up to three tumors, each under 3 cm, with no spread to blood vessels. If your tumor is bigger or has invaded veins, you’re usually out-unless you’ve had successful treatment that shrinks it and lowers your alpha-fetoprotein (AFP) level below 500. Even then, you need special approval.
Other conditions block you outright. Active infections, advanced heart or lung disease, or cancer that’s spread beyond the liver are absolute no-gos. Mental health matters too. If you can’t manage your meds or don’t have someone to help you after surgery, the team may hold off. You need a support system. Stable housing. Reliable transportation. A plan for follow-up care. The transplant team doesn’t just look at your liver-they look at your whole life.
How the Surgery Works
The surgery itself is a marathon. It takes between six and twelve hours. Most patients get the “piggyback” technique, where the surgeon removes the diseased liver but keeps the big vein (inferior vena cava) intact. This reduces blood loss and speeds up recovery. The donor liver is stitched into place-arteries, veins, and bile ducts all reconnected.There are two kinds of donors: deceased and living. Most livers come from people who’ve died and donated their organs. But living donation is growing. A healthy person can give part of their liver-usually the right lobe, which makes up about 60% of the organ. The liver regenerates in both donor and recipient. Donors typically stay in the hospital for a week and need six to eight weeks to feel normal again. The risk? Less than 0.2% die. About 20-30% have complications like bile leaks or infections.
Living donation cuts waiting time. For someone with a MELD score over 25, waiting for a deceased donor can take over a year. With a living donor, it’s often three months or less. That’s life-saving. But not everyone has a willing donor. And not every donor is medically perfect. New guidelines now allow donors with controlled high blood pressure and BMI up to 32, based on recent data showing similar outcomes to healthier donors.
Another shift is happening with organs from donors after circulatory death (DCD). These are hearts that stopped beating before donation. In 2022, 12% of liver transplants came from DCD donors. They used to have higher complication rates, especially with bile ducts. But now, machines that pump oxygenated fluid through the liver (machine perfusion) are cutting those complications by nearly a third. The FDA approved the first portable perfusion device in June 2023, letting organs stay viable for up to 24 hours instead of 12.
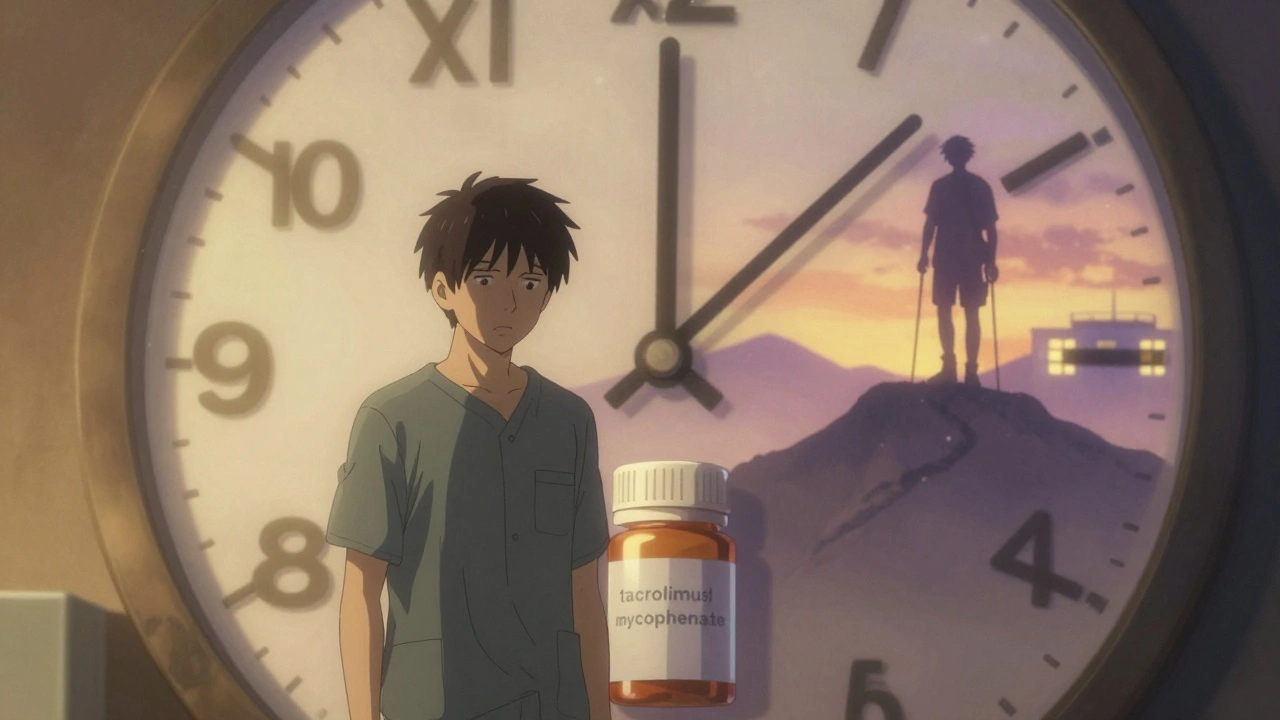
Life After the Transplant: Immunosuppression
Your new liver isn’t yours. Your body sees it as an invader. That’s why you need immunosuppressants-drugs that trick your immune system into leaving the organ alone.Right after surgery, most patients get a one-time IV dose of basiliximab or anti-thymocyte globulin. Then, they start lifelong daily pills. The standard combo is tacrolimus, mycophenolate, and a steroid like prednisone. Tacrolimus is the backbone. Doctors aim for blood levels between 5 and 10 ng/mL in the first year, then lower it to 4-8. Too low? Rejection. Too high? Kidney damage, tremors, or diabetes.
Side effects are real. About 35% of patients develop kidney problems within five years. One in four gets diabetes. One in five has nerve issues like shaking or trouble sleeping. Mycophenolate causes nausea, diarrhea, or low blood counts in up to a third of people. Prednisone adds weight gain, bone thinning, and mood swings. That’s why 45% of U.S. transplant centers now skip prednisone after the first month. They use higher doses of tacrolimus and mycophenolate instead-and cut diabetes risk from 28% to 17%.
Rejection still happens. About 15% of patients have at least one episode in the first year. It’s often caught early through blood tests. The fix? Increase tacrolimus or add sirolimus. Most patients never have another episode after that.
Monitoring is relentless. Weekly blood tests for the first three months. Then every two weeks. Then monthly. After a year, it’s quarterly. You’ll need a liver biopsy if your enzymes spike. You’ll learn to recognize warning signs: fever over 100.4°F, yellow skin, dark urine, extreme fatigue. Call your team immediately. A delay can mean losing the graft.

Cost, Access, and Inequality
A liver transplant costs $500,000 to $1 million in the first year. Medications alone run $25,000 to $30,000 per year-forever. Insurance often covers it, but many patients get denied pre-transplant evaluations. One 2023 survey found 32% of candidates faced coverage denials.Where you live affects your odds. In the Midwest (OPTN Region 2), someone with a MELD score of 25-30 waits about eight months. In California (Region 9), it’s 18 months. In the Southwest (Region 5), you’re 40% less likely to get a liver within 90 days than someone with the same score in the Mid-Atlantic. These gaps aren’t random. They’re built into how organs are allocated across regions.
Some places are trying to fix this. British Columbia changed its rules in November 2025 to better serve Indigenous patients. They now include cultural support in psychosocial evaluations and adjust sobriety timelines based on community needs, not rigid deadlines. Other centers are testing whether three months of abstinence is enough for alcohol-related liver disease. Early data shows survival rates are nearly the same as with six months.
What Happens Long-Term?
Most people go back to work, travel, and live full lives. Five-year survival is around 70%. Many live 20 years or more. But it’s not easy. You’ll take pills every day. You’ll avoid crowds during flu season. You’ll never skip a lab test. You’ll need annual skin checks-immunosuppressants raise your cancer risk.There’s hope on the horizon. Researchers at the University of Chicago have helped 25% of pediatric transplant recipients stop all immunosuppression by age five using a therapy that boosts regulatory T-cells. It’s not ready for adults yet, but it’s a glimpse of a future where rejection isn’t permanent.
Artificial livers? They’re still just bridges. No device has kept someone alive more than 30 days without a transplant. That’s why liver transplantation remains the gold standard. It’s not perfect. It’s not fair. But for now, it’s the only thing that gives people with failed livers a real shot at tomorrow.
What You Need to Know Before You Start
If you’re considering a transplant, here’s what to do:- See a hepatologist. Get your MELD score calculated.
- Find a transplant center near you. Call and ask about their waiting times and donor criteria.
- Start sobriety if you drink. Document it. Get counseling.
- Build your support system. Who will drive you to appointments? Who will help with meds?
- Check your insurance. Ask what’s covered before and after transplant.
- Ask about living donation. Talk to family. Even if they say no now, keep the conversation open.
- Learn your meds. Know what each pill does. Know the side effects.
- Join a patient group. Reddit’s r/liverdisease has real stories. You’re not alone.
Can you live a normal life after a liver transplant?
Yes, most people return to work, travel, and enjoy family life. But you’ll always need to take immunosuppressants, attend regular checkups, and avoid infections. You can’t drink alcohol, and you’ll need to be careful with medications and supplements. With proper care, many live 20+ years after transplant.
How long is the waiting list for a liver transplant?
It varies by region and MELD score. For someone with a score of 25-30, wait times range from 8 months in the Midwest to 18 months in California. With a living donor, you can skip the wait entirely-often getting transplanted within 3 months.
What happens if you reject the new liver?
Acute rejection happens in about 15% of patients in the first year. It’s usually caught early through blood tests and treated by adjusting immunosuppressant doses. Most patients recover fully. Chronic rejection is rarer but harder to treat. It can lead to graft failure, requiring another transplant.
Can you donate part of your liver if you’re over 55?
Standard age limits are 18-55, but exceptions exist. Some centers have successfully transplanted livers from donors in their 60s if they’re in excellent health, have no liver disease, and pass all medical tests. The key is liver quality and anatomy-not just age.
Why is sobriety required before a liver transplant?
Alcohol use increases the risk of damaging the new liver and makes it harder to follow complex care plans. The six-month rule was based on early data showing better outcomes. But newer studies show patients with three months of sobriety have similar survival rates. Some centers are changing policies to reflect this, especially if the patient is in therapy and has strong support.
How much do liver transplant medications cost each year?
Annual medication costs range from $25,000 to $30,000, not including doctor visits, labs, or complications. Insurance usually covers most of it, but copays and deductibles can still add up. Some drug manufacturers offer patient assistance programs to help with out-of-pocket costs.
What Comes Next?
If you’re on the list, keep your body strong. Eat well. Walk daily. Don’t skip your appointments. If you’re thinking about donating, talk to your doctor. Learn what’s involved. The liver is the only organ that regenerates. That’s why it’s possible to give part of yours-and save someone else’s life.Transplant isn’t the end of the story. It’s the start of a new one. A harder one, maybe. But one with more tomorrows.

Reshma Sinha
December 13, 2025 AT 02:10Wow, this is such a comprehensive breakdown! The MELD score dynamics are critical, but I’m especially impressed by the shift toward three-month sobriety protocols-this aligns with recent hepatology guidelines from EASL 2023. The data on living donor outcomes with BMI up to 32? Game changer. We need more centers adopting this. Also, machine perfusion for DCD livers is no longer experimental-it’s standard of care now. The FDA’s 24-hour portable device approval? Huge leap forward for equity in organ allocation.
Lawrence Armstrong
December 14, 2025 AT 05:33So many people don’t realize how much prep happens before surgery. Like, you’re not just waiting-you’re training your body, building your support crew, learning your meds. I’ve seen patients crash because they thought ‘getting listed’ was the finish line. Nope. It’s the starting gate. 🤝
wendy b
December 15, 2025 AT 12:56Actually, the MELD score is kinda outdated. It doesn't account for sarcopenia or frailty, which are huge predictors of post-op mortality. And the 6-month sobriety rule? Total arbitrary bs. I read a paper in JHEP Reports last month showing 3-month abstinence had identical 5-year survival. Some centers are just clinging to dogma. Also, why is prednisone still used at all? It's 2025.
Donna Anderson
December 15, 2025 AT 21:00Yessss! This is exactly what I needed to hear before my consult. I’ve been sober for 4 months and was terrified I wouldn’t qualify. So glad to hear some places are changing. Also, living donor stuff gave me hope-my cousin is gonna get tested tomorrow 😭❤️
Levi Cooper
December 17, 2025 AT 05:01Let’s be real-why are we giving livers to people who drank themselves into failure? I work hard my whole life, pay taxes, never touched a drink, and now I’m supposed to wait behind someone who chose to destroy their liver? This system is broken. We should prioritize those who didn’t cause their own demise. It’s not rocket science.
sandeep sanigarapu
December 17, 2025 AT 09:34Transplant is not merely medical. It is social, psychological, economic. The system must recognize that. In India, we have families who sell land to pay for post-op care. In America, insurance denials are common. The MELD score is objective. But access? Not at all. We must fix the gap between eligibility and actual care.
nikki yamashita
December 18, 2025 AT 09:46OMG I’m crying. My brother got his transplant last year. He’s back to coaching soccer now. The meds are rough but worth it. I’m so glad someone finally wrote this without sugarcoating. Also-YES to skipping prednisone! He’s been off it for 8 months and no diabetes yet 🙌
Adam Everitt
December 19, 2025 AT 03:13It’s fascinating how the liver, this ancient, resilient organ, becomes the crucible for modern ethics: who deserves life? Who’s worthy? We measure sobriety in months, but what of trauma? Addiction as self-medication? The system reduces complexity to numbers-but the body remembers what the spreadsheet forgets.
Rob Purvis
December 20, 2025 AT 23:11Can we talk about the cost? $25K–$30K per year in meds? That’s insane. And the fact that 32% of candidates get denied pre-transplant evals? That’s systemic failure. Also, the regional disparities? Why is someone in California waiting twice as long as someone in Ohio with the same MELD? The UNOS algorithm needs a total overhaul. We’re rationing life based on zip code. That’s not healthcare-that’s geography-based discrimination.
Ashley Skipp
December 22, 2025 AT 19:37People think transplant is a cure. It’s not. It’s a life sentence with pills. And don’t even get me started on the skin cancer risk. I’ve had 17 biopsies in 4 years. You’re never done. You’re just waiting for the next failure.
Nathan Fatal
December 23, 2025 AT 06:14The most profound thing here isn’t the surgery or the drugs-it’s the regeneration. The liver is the only organ that rebuilds itself. That’s why living donation works. That’s why we can give part of ourselves and survive. Maybe the lesson isn’t just medical-it’s metaphorical. We are capable of renewal. Even when broken, we can grow back stronger-if given the chance.
Robert Webb
December 25, 2025 AT 04:06I’ve been on the list for 14 months. I’m 58. I’ve been sober for 8 months. I had a living donor lined up, but they had a benign cyst. The team said it was too risky. I’m still waiting. But I’ve learned so much. I walk 5 miles a day. I track my sodium. I’ve joined a support group. I’ve learned to read my labs. I’ve become an expert in tacrolimus trough levels. This isn’t just survival-it’s a second education. And I’m grateful. Even now. Even while waiting.
Laura Weemering
December 25, 2025 AT 04:22Okay but… what if you’re just… tired? What if you don’t want to take pills forever? What if you’re tired of being a ‘transplant patient’? What if you just want to be… normal? Is that selfish? I’ve been told I’m ‘ungrateful’ for feeling this way. But I’m not ungrateful. I’m exhausted. And nobody talks about that.