Pediatric Medication Dosing: How to Calculate Weight-Based Doses Accurately
Getting the right dose of medicine for a child isn’t about age. It’s not about how tall they are. It’s not even about what the bottle says. It’s about their weight. A 10-pound baby and a 60-pound toddler might both be labeled as ‘toddlers,’ but giving them the same dose could be deadly. That’s why weight-based dosing isn’t just a best practice-it’s the only safe way to give medications to children.
Why Weight Matters More Than Age
Imagine two 3-year-olds. One weighs 25 pounds. The other weighs 45 pounds. That’s nearly double the body weight. If you gave both the same dose of antibiotics based on age alone, the lighter child might get too much and get sick. The heavier child might get too little and not get better. This isn’t hypothetical. It happens. In fact, dosing errors are the number one cause of medication mistakes in kids. The American Academy of Pediatrics and the Institute for Safe Medication Practices both say the same thing: use weight. Not age. Not guesswork. Not ‘a teaspoon for toddlers.’ A child’s body processes drugs differently based on how much they weigh. Their liver and kidneys aren’t fully developed, so even small errors can lead to serious harm. A 2021 case study in the Journal of Pediatric Pharmacology and Therapeutics reported a 15-kilogram child who received 10 times the correct dose of amoxicillin because the nurse confused pounds and kilograms. The child ended up in the hospital with severe vomiting and dehydration. That kind of error is preventable.The Basic Math: mg/kg Explained
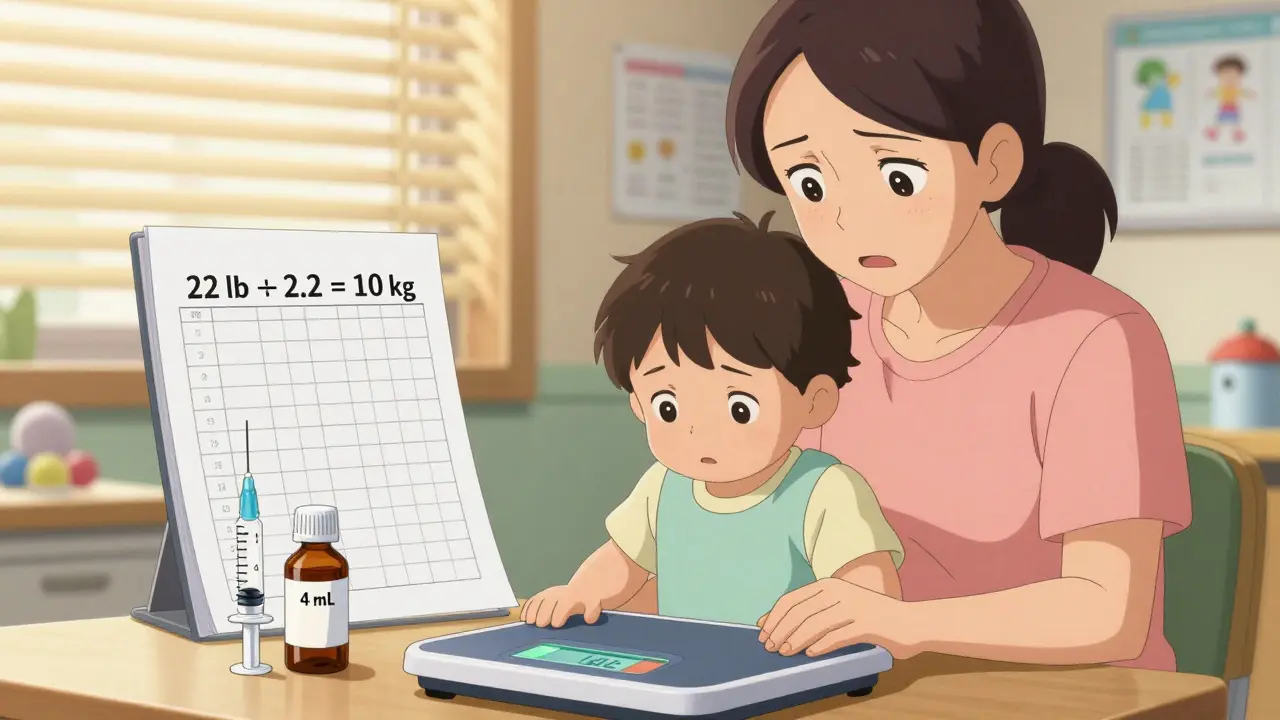
Most pediatric medications are dosed in milligrams per kilogram (mg/kg). That means for every kilogram of body weight, the child gets a certain number of milligrams of medicine. It sounds simple, but it’s where most mistakes happen. Let’s break it down:- Get the child’s weight in kilograms (kg). If it’s in pounds (lb), convert it. Use 1 kg = 2.2 lb. No exceptions.
- Multiply the weight in kg by the prescribed dose in mg/kg.
- Figure out how much liquid or tablet that equals.
Common Mistakes That Can Kill
Here’s the scary part: 80% of all pediatric dosing errors involve unit conversion mistakes. That’s right-most of the time, it’s not the math. It’s not knowing that 1 kg equals 2.2 lb. Nurses, parents, even pharmacists have given the wrong dose because they used pounds instead of kilograms. Another big problem? Confusing ‘mg/kg/day’ with ‘mg/kg/dose.’ If a prescription says ‘5 mg/kg/day’ and you give it all at once, you’re overdosing. It has to be split. Always ask: Is this the total daily dose? Or the amount per dose? And don’t forget concentration. Acetaminophen comes in different strengths: 160 mg/5 mL for children and 500 mg/5 mL for adults. If you use the adult concentration for a child, you’re giving five times too much. A 2023 study from St. Louis Children’s Hospital found that 65% of parental dosing errors happened because they mixed up these formulations.
When Weight Isn’t Enough: BSA and Special Cases
For some drugs-especially chemotherapy, anticonvulsants, or immunosuppressants-weight alone isn’t enough. These drugs have very narrow safety margins. Too little won’t work. Too much can be toxic. That’s where Body Surface Area (BSA) comes in. BSA is calculated using height and weight. The Mosteller formula is the standard: √(height in cm × weight in kg ÷ 3600). For a child who is 97 cm tall and weighs 16.8 kg, the BSA is 0.67 m². The dose is then given in mg per m². This isn’t something parents need to do at home. But it’s critical for hospital settings. Vincristine, for example, is always dosed by BSA. Even small errors here can lead to nerve damage or organ failure. Some medications also have weight caps. Buprenorphine, used for pain in older children, is capped at 0.4 mg/kg/hour-even if the child weighs more than 50 kg. Giving more won’t help and could cause breathing problems.Double-Check Protocols Save Lives
In hospitals, no pediatric dose is given without two people checking it. One calculates. The other verifies. This isn’t bureaucracy-it’s survival. Studies show that double-checking reduces dosing errors by up to 70%. Electronic health records (EHRs) like Epic and Cerner now automatically convert pounds to kilograms and calculate doses based on weight. But they’re not foolproof. If the weight is entered wrong, the computer will give the wrong answer-and everyone will trust it. That’s why best practices include:- Always measure weight, never estimate.
- Record both pounds and kilograms in the chart.
- Write doses as ‘mg/kg’ with clear frequency (e.g., ‘5 mg/kg every 8 hours’ not ‘5 mg/kg/d’).
- Verify concentration on the medication label every single time.
- Never give Benadryl to children under 2 years unless a doctor says so-no exceptions.

What Parents Need to Know
If you’re giving medicine at home, you’re responsible for getting it right. Don’t guess. Don’t rely on old bottles or memory. Here’s what to do:- Always weigh your child if possible. Use a baby scale or visit the pharmacy.
- Convert pounds to kilograms: divide by 2.2.
- Check the label for concentration. Is it 160 mg/5 mL or 250 mg/5 mL? Write it down.
- Use the dosing syringe that comes with the medicine. Never use a kitchen spoon.
- If the prescription says ‘mg/kg/day,’ ask: ‘How many times a day do I give it?’
- If you’re unsure, call the doctor or pharmacist. It’s better to ask than to risk it.
The Bigger Picture: Safety Systems Are Changing
The medical world is finally catching up to how dangerous pediatric dosing errors are. The Joint Commission lists improper pediatric dosing as a National Patient Safety Goal. The FDA now requires drug labels to include pediatric dosing data. The Institute for Safe Medication Practices is pushing to ban abbreviations like ‘mg/kg/d’ because they’re too confusing. New tools are coming. Children’s Hospital of Philadelphia is testing AI that flags unusual doses by comparing them to thousands of past cases. Early results show it catches 92% of potential errors before they happen. But technology alone won’t fix this. People still have to do the math, read the labels, and ask questions. The best system in the world won’t help if someone enters the wrong weight or misreads a concentration.Final Rule: When in Doubt, Stop
No dose is so urgent that you can’t pause and check. If the number feels wrong-if the volume seems too big, the dose too high, the frequency too frequent-stop. Call the prescriber. Ask again. Verify the math. Your child’s life depends on it. Weight-based dosing isn’t complicated. It’s just precise. And precision saves lives.How do I convert my child’s weight from pounds to kilograms?
Divide the weight in pounds by 2.2. For example, if your child weighs 33 pounds, divide 33 by 2.2 to get 15 kg. Never round until the final step. Always use the full number during calculation to avoid errors.
What if the prescription says ‘mg/kg/d’?
That’s not a standard notation and is dangerously ambiguous. ‘d’ could mean ‘day’ or ‘dose.’ Always call the prescriber to clarify whether it’s total daily dose or per dose. Never assume. Many medication errors come from this exact confusion.
Can I use the same dosing for different brands of the same medicine?
No. Different brands of acetaminophen, ibuprofen, or antibiotics often have different concentrations. One might be 160 mg/5 mL, another 250 mg/5 mL. Always check the label. The dose in mL will change even if the total mg stays the same.
Is it safe to use a kitchen teaspoon to measure medicine?
Never. Kitchen spoons vary in size. A teaspoon might hold 3 mL or 7 mL. Always use the dosing syringe or cup that comes with the medicine. These are calibrated for accuracy.
Why can’t I just give my child half of an adult dose?
Children aren’t small adults. Their bodies absorb, process, and eliminate drugs differently. A half adult dose might be too much for a toddler or too little for a teenager. Weight-based dosing accounts for these differences. Clark’s Rule (adult dose × child’s weight in lb ÷ 150) is outdated and inaccurate for most medications.
What should I do if I think I gave the wrong dose?
Call your pediatrician or poison control immediately. Do not wait for symptoms. In the U.S., call 1-800-222-1222. Have the medicine bottle, your child’s weight, and the amount given ready. Quick action can prevent serious harm.

Jane Lucas
December 27, 2025 AT 20:12my kid got the wrong dose once and i still panic when i open the medicine bottle. i dont even trust the pharmacy anymore. just write the weight in kg on the bottle myself now. no exceptions.
dean du plessis
December 28, 2025 AT 05:12good post. i work in a clinic in cape town and we see this all the time. parents using teaspoons because they dont have a syringe. we give them free ones now. simple fix. big difference.
Caitlin Foster
December 29, 2025 AT 19:59OH MY GOD. I JUST REALIZED I DID THIS LAST MONTH. 😭 I used the adult Tylenol because it was ‘close enough’ and my 3-year-old was screaming. I’m calling my pediatrician right now. THANK YOU FOR THIS. I’m printing this out and taping it to the fridge. Someone save me from my own dumbassery.
Miriam Piro
December 31, 2025 AT 08:37they don’t want you to know this but weight-based dosing is just the tip of the iceberg. the real danger? the pharmaceutical companies push the same syrup for every kid because it’s cheaper. they know parents won’t check the concentration. they know nurses are overworked. they know the EHRs auto-fill the wrong units. this isn’t negligence - it’s systemic. they profit from your ignorance. every time you use a kitchen spoon, you’re feeding the machine. and they’re laughing. 💀
Kylie Robson
December 31, 2025 AT 23:51the most critical oversight in this entire framework is the failure to account for pharmacokinetic variability in pediatric populations. while mg/kg is the standard, the volume of distribution, clearance rates, and protein binding coefficients are ontogenically dynamic and non-linear across developmental stages. without adjusting for gestational age-adjusted weight in neonates or lean body mass in obese pediatric patients, even ‘accurate’ dosing remains pharmacologically inappropriate. furthermore, the use of Mosteller’s formula assumes normal body composition - which fails catastrophically in children with malnutrition or edema. the current guidelines are fundamentally reductionist.
James Bowers
January 1, 2026 AT 01:55This is an egregious oversimplification of pediatric pharmacology. The reliance on weight alone disregards the profound influence of hepatic enzyme maturation, renal glomerular filtration rate development, and blood-brain barrier permeability across infancy and childhood. The assertion that ‘precision saves lives’ is misleading - it is systemic protocol, standardized labeling, and mandatory double-checks that save lives. This post reads like a pamphlet for a pharmacy intern. The real problem? Inadequate training, not patient weight.
Kishor Raibole
January 1, 2026 AT 08:14It is with the utmost gravity that I must express my profound concern regarding the casual tone adopted in this discourse. The normalization of colloquialisms such as ‘don’t guess’ and ‘call the doctor’ undermines the solemn responsibility inherent in pediatric therapeutics. The administration of pharmaceuticals to minors is not a matter of informal advice, but a sacred covenant between the medical profession and the sanctity of life. I implore the author to consider the dignity of the subject matter and elevate the discourse accordingly.
Elizabeth Alvarez
January 3, 2026 AT 06:18you think this is about weight? no. it’s about the FDA and the AMA working together with Big Pharma to control the population. they want you to be dependent on their ‘correct’ dosing because if you knew how to do it yourself, you’d realize how many of these meds are unnecessary. why do they even sell pediatric amoxicillin in 250mg/5mL? why not just 160? because they want you to make a mistake. they want you to panic. they want you to come back. they want you to trust them. they’ve been doing this since the 80s. remember when they said fluoride was safe? now look. they’re lying. always. always. always. i’ve seen the documents. they know. they just don’t care. your child’s liver is a test subject. you’re just the delivery system.
Chris Garcia
January 4, 2026 AT 14:20In my village in Nigeria, we use the palm of the hand to measure medicine - one palm for infants, two for toddlers. It’s not perfect, but it’s trusted. We don’t have scales or syringes. We have mothers who know their children’s faces when they’re sick. Maybe the real lesson here isn’t about math - it’s about presence. When you’re there, when you watch, when you feel the fever in their skin - you don’t need a calculator. You need love. And sometimes, love knows the dose better than the label.
Jane Lucas
January 5, 2026 AT 15:14that one comment about the syrup concentration? yeah. i did that. i gave my kid the adult one. i thought it was the same. i didn’t even realize until i saw the bottle next to the one from last year. i cried. i called poison control. they said she’d be fine. but i still check every bottle twice now. no shame. just survival.