REMS Programs Explained: How the FDA Manages High-Risk Drug Safety
When a drug can save lives but also cause serious harm-like birth defects, organ failure, or deadly blood disorders-the FDA doesn’t just approve it and walk away. Instead, it puts in place a strict safety system called a REMS program. These aren’t optional guidelines. They’re legally required safeguards designed to make sure the benefits of a dangerous drug outweigh its risks. For patients, prescribers, and pharmacists, REMS can mean extra steps, paperwork, and delays. But they’re also the reason some life-saving drugs are even available at all.
What Exactly Is a REMS Program?
REMS stands for Risk Evaluation and Mitigation Strategy. It’s a formal plan the U.S. Food and Drug Administration (FDA) can require for certain prescription drugs with serious safety risks. The FDA gained the legal power to enforce REMS in 2007 under the Food and Drug Administration Amendments Act (FDAAA). Before that, safety controls were patchy-like the strict pregnancy prevention program for isotretinoin (Accutane) in the 1980s, or the blood monitoring needed for clozapine, a drug used for treatment-resistant schizophrenia.
Today, REMS programs are used for about 185 drugs, covering roughly 5.7% of all prescription medications in the U.S. The highest concentration is in oncology and hematology. Drugs like lenalidomide (Revlimid), pomalidomide (Pomalyst), and alemtuzumab (Lemtrada) all have complex REMS because they can cause severe birth defects, bone marrow failure, or dangerous immune reactions.
The goal isn’t to block access-it’s to control risk. As FDA pharmacist Dr. Kimberly Chiu says, REMS lets patients get drugs they need, while reducing the chance of harm. Without REMS, many of these drugs would never get approved.
The Four Main Parts of a REMS Program
Not every REMS is the same. But all include at least one of two core components: a Medication Guide or a patient package insert. These are printed handouts given to patients that explain the drug’s risks in plain language. About 78% of REMS programs require these guides.
The other three components are added based on how serious the risk is:
- Communication Plans: These are targeted messages to doctors and pharmacists. They might come as letters, emails, or training materials. About 62% of REMS programs use these to make sure prescribers understand the dangers and how to manage them.
- Elements to Assure Safe Use (ETASU): This is the strictest level. About 45% of REMS programs have ETASU. It can include:
- Prescriber certification-doctors must complete training and register before they can write the prescription.
- Pharmacy certification-only certain pharmacies, often specialty ones, can dispense the drug.
- Restricted distribution-patients can only get the drug in hospitals or clinics, not regular pharmacies.
- Patient enrollment-patients must sign up in a registry so their use is tracked.
- Monitoring requirements-like monthly blood tests or pregnancy tests before each dose.
For example, the Revlimid REMS program requires every prescriber to be certified, every patient to enroll in a registry, and women of childbearing age to have two negative pregnancy tests before each prescription. That’s not just paperwork-it’s a full workflow change for oncology clinics.
Who Runs and Pays for REMS?
The drug manufacturer is legally responsible for designing, funding, and running the REMS program. That’s not cheap. On average, each REMS costs a company $2.7 million per year. For drugs with ETASU, costs go even higher because of staffing, software, training, and audits.
Healthcare providers also pay a price. Doctors must complete certification, which takes about 45 minutes per REMS program. Pharmacists spend extra time verifying prescriber status, checking patient enrollment, and logging data. One pharmacist on Reddit said the Entyvio REMS adds 15-20 minutes per prescription just to check the online portal.
Specialty pharmacies handle 89% of REMS drugs because they have the systems and staff to manage the extra steps. But even they struggle. A 2023 survey found only 32% of infusion centers felt the FDA’s REMS support materials were helpful enough.
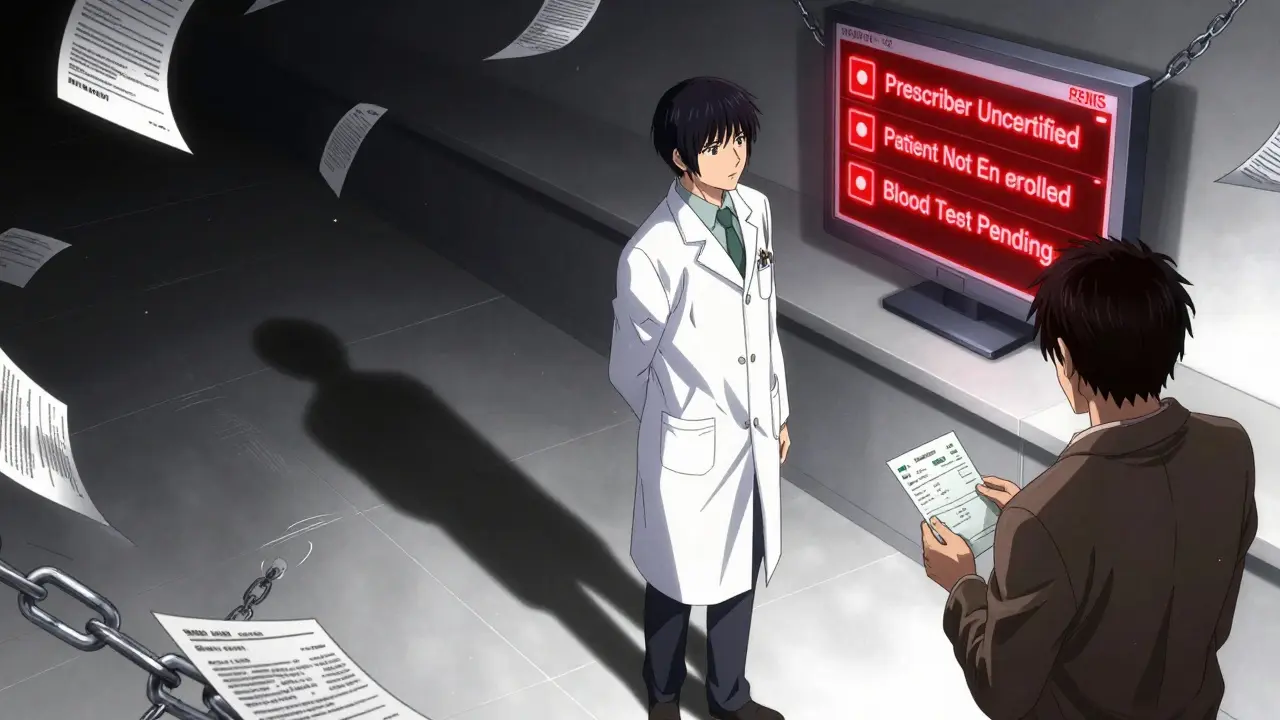
Why REMS Can Delay Treatment
For patients, REMS can mean waiting days-or weeks-for a prescription to be filled. A GoodRx survey in 2023 found 42% of patients on REMS drugs experienced delays. Reasons? Missing certification paperwork, pharmacy not enrolled, or waiting for test results.
One of the worst cases is Lemtrada, used for multiple sclerosis. It requires administration in a hospital, daily blood tests for months, and a long monitoring period after each infusion. Patients often need to travel far, take time off work, and schedule multiple appointments just to get one dose.
Another hidden problem: generic drug delays. A 2024 Health Affairs study found that 78% of generic manufacturers faced REMS-related delays averaging 14.3 months before they could bring their versions to market. Why? Brand-name companies control access to drug samples needed for testing, and REMS rules make it harder to get them. This keeps prices high and limits patient choice.
How REMS Is Changing-And Why It Matters
The FDA knows REMS can be burdensome. That’s why they launched the REMS Modernization Initiative in 2023. The goal? Make it simpler without sacrificing safety.
Here’s what’s coming:
- Standardized forms and digital certification-no more paper logs or separate portals for each drug.
- A new REMS Dashboard by Q3 2025 that shows real-time data on how well each program is working.
- Electronic verification of patient enrollment and testing results, cutting down on manual checks.
- A new REMS Assessment Standard by December 2025, required by the 21st Century Cures Act Reauthorization.
Experts like Dr. Rachel Sherman, former FDA deputy commissioner, believe future REMS will use real-world data-like electronic health records and pharmacy claims-to monitor safety automatically, instead of relying on manual reporting.
Some REMS have already been removed. Only three since 2007. The most recent was Zeposia for multiple sclerosis, pulled in March 2023 after the FDA determined its safety risks were well-managed through regular labeling.
What Patients and Providers Should Do
If you’re prescribed a drug with a REMS:
- Ask your doctor: “Is there a REMS for this? What do I need to do?”
- Make sure your pharmacy is certified to dispense it.
- Keep copies of all certifications, test results, and enrollment confirmations.
- If you’re delayed, contact the drug manufacturer’s REMS support line-they’re required to help.
For prescribers and pharmacists:
- Use the FDA’s REMS@FDA website to check if a drug has an active REMS.
- Bookmark the certification portals for drugs you prescribe often.
- Advocate for electronic integration-paper systems are outdated and error-prone.
REMS isn’t perfect. It’s slow, expensive, and confusing. But it works. It’s the reason a drug like thalidomide-once infamous for causing birth defects-is now safely used to treat leprosy and multiple myeloma. The system isn’t broken. It just needs to catch up to the digital age.
What drugs require a REMS program?
Drugs with serious, life-threatening risks often require REMS. These include medications that can cause severe birth defects (like lenalidomide and thalidomide), life-threatening blood disorders (like clozapine), or serious immune reactions (like alemtuzumab). The FDA maintains a public list of all active REMS programs on the REMS@FDA website, which includes over 120 programs covering about 185 drugs. Most are in oncology, neurology, and autoimmune conditions.
Can a REMS program be removed?
Yes, but it’s rare. The FDA can remove a REMS if evidence shows the drug’s risks are well-managed through standard labeling or if the program doesn’t improve safety. Since 2007, only three REMS programs have been fully discontinued. The most recent was Zeposia in March 2023, after the FDA determined its safety profile could be managed without the extra requirements.
Why do REMS programs delay generic drugs?
Brand-name manufacturers control access to drug samples needed for generic companies to test bioequivalence. REMS rules often restrict who can receive those samples, and the process to get them can take over a year. A 2024 study found 78% of generic manufacturers faced delays averaging 14.3 months because of REMS. This limits competition and keeps prices high. Legislative changes are now being proposed to fix this.
Do REMS programs actually prevent harm?
Yes. The FDA estimates REMS programs prevent $8.4 billion in healthcare costs each year by avoiding serious adverse events like birth defects, organ failure, or fatal infections. While they add administrative work, the data shows they reduce harm. For example, the isotretinoin REMS reduced birth defects by over 90% after its implementation. The cost-$1.2 billion annually-is considered a necessary trade-off.
How can patients get help with REMS requirements?
Each REMS program has a dedicated support line and website managed by the drug manufacturer. Patients can call for help with certification, enrollment, or finding a certified pharmacy. The FDA also provides educational materials on the REMS@FDA website. If delays persist, patients should ask their doctor to contact the manufacturer’s REMS coordinator-manufacturers are legally required to assist.

Peyton Feuer
January 4, 2026 AT 14:12Akshaya Gandra _ Student - EastCaryMS
January 5, 2026 AT 05:23Dee Humprey
January 6, 2026 AT 16:04Michael Rudge
January 7, 2026 AT 15:06Joseph Snow
January 8, 2026 AT 21:29Jennifer Glass
January 10, 2026 AT 17:23Jacob Milano
January 11, 2026 AT 19:38melissa cucic
January 12, 2026 AT 20:00en Max
January 14, 2026 AT 17:10Terri Gladden
January 16, 2026 AT 15:36Enrique González
January 17, 2026 AT 17:59saurabh singh
January 18, 2026 AT 07:18Rory Corrigan
January 18, 2026 AT 08:36Angie Rehe
January 18, 2026 AT 14:25John Wilmerding
January 19, 2026 AT 22:54