Residronate and Bone Metabolism: How This Drug Shapes Bone Health
Fracture Risk Reduction Calculator
Calculate estimated vertebral fracture risk reduction with Residronate based on clinical evidence showing 30-40% fracture reduction after 3 years of use.
When doctors treat osteoporosis, Residronate is a synthetic bisphosphonate that binds to bone surface and slows down bone resorption. It was approved in 2022 and is prescribed for patients with high fracture risk. Understanding why it works requires a quick look at how bone constantly renews itself.
Key Takeaways
- Residronate belongs to the bisphosphonate class and targets osteoclast activity.
- It boosts bone mineral density (BMD) by limiting bone breakdown while allowing formation to continue.
- Clinical trials show a 30‑40% reduction in vertebral fractures after three years of use.
- Side‑effects are mostly mild gastrointestinal issues; rare cases of atypical femur fractures can occur with long‑term use.
- Choosing between Residronate and other agents depends on dosing convenience, kidney function, and individual risk profile.
What Is Residronate?
Residronate is a nitrogen‑containing bisphosphonate, chemically similar to alendronate and risedronate. Its structure includes a phosphonate group that has high affinity for hydroxyapatite, the mineral component of bone. Once attached, it stays in the bone matrix for years, releasing slowly as bone remodels.
Typical dosing is a weekly oral tablet of 35 mg, taken on an empty stomach with plenty of water. The drug is not suitable for patients with severe renal impairment (eGFR < 30 mL/min) because it is cleared unchanged by the kidneys.
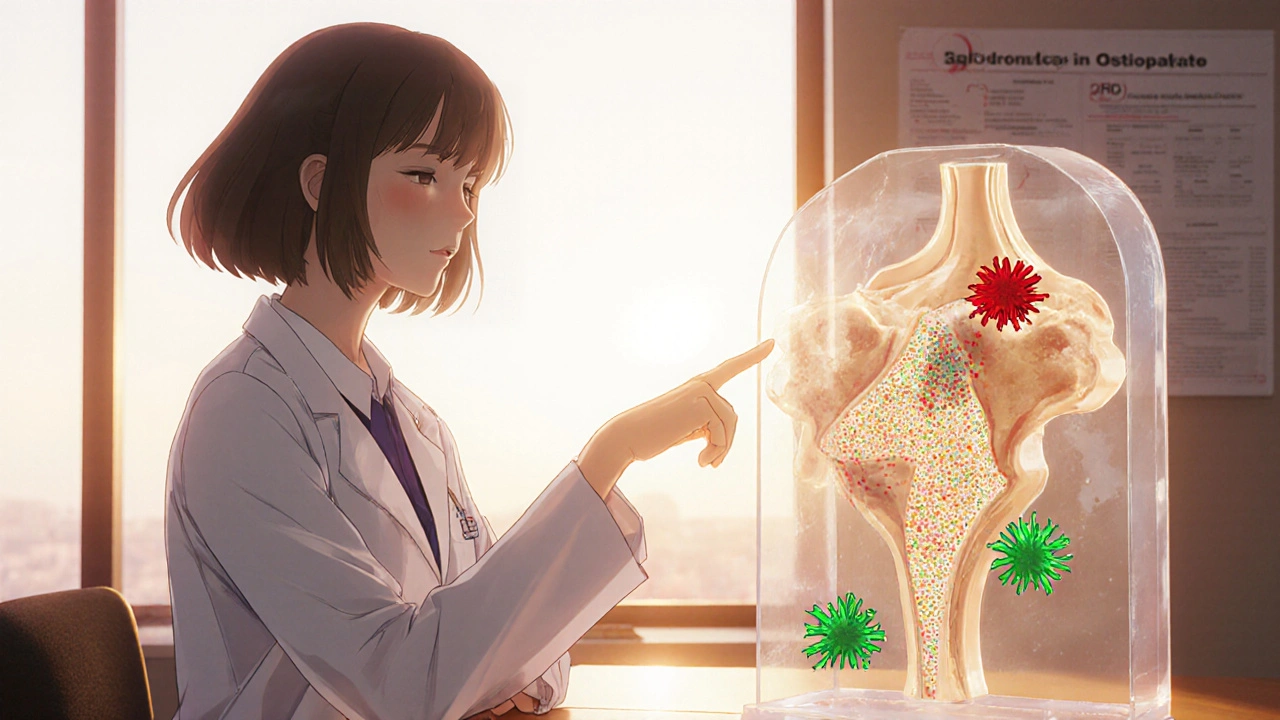
How Bone Metabolism Works
Bone is a living tissue that undergoes continuous turnover through two main cell types: osteoclasts that break down old bone and osteoblasts that lay down new matrix. This process is tightly regulated by hormones such as parathyroid hormone (PTH) and vitamin D, and by signaling molecules like RANKL (receptor activator of nuclear factor‑κB ligand).
When the balance tips toward resorption, bone density falls, making fractures more likely. Osteoporosis is essentially a state of excessive osteoclast activity relative to osteoblast formation.
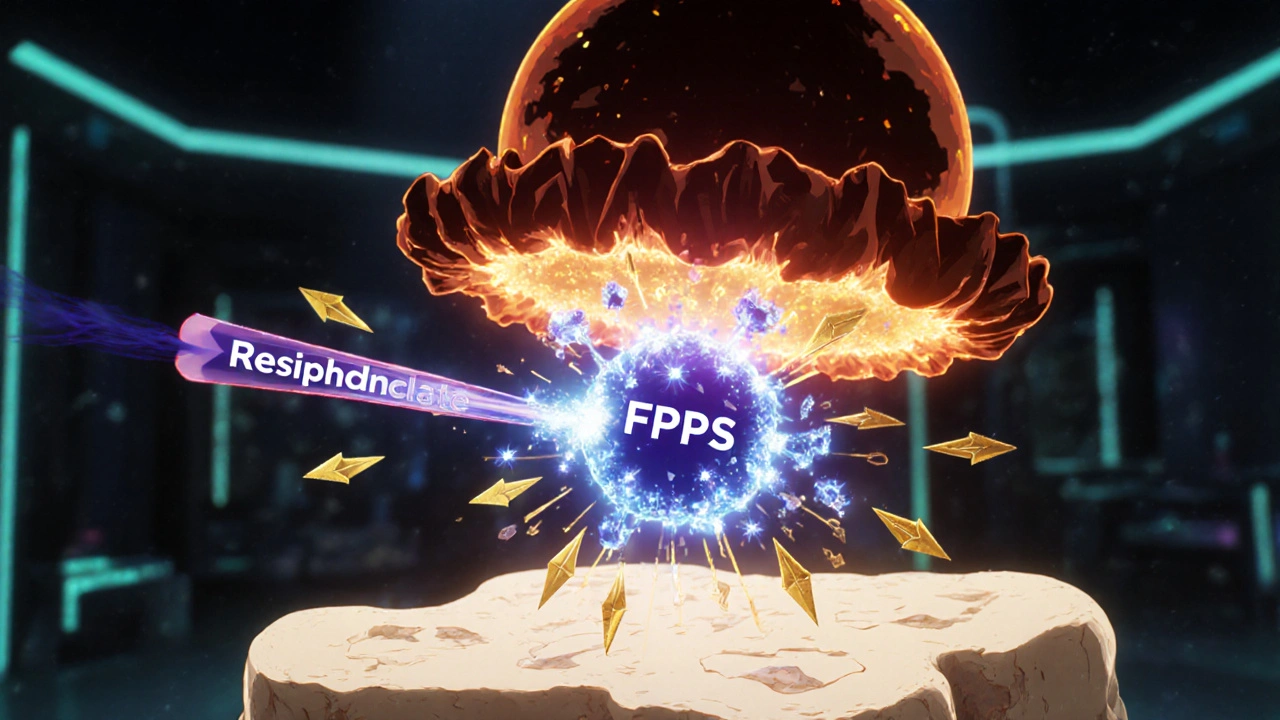
Mechanism of Action of Residronate
Residronate inhibits the enzyme farnesyl pyrophosphate synthase (FPPS) within the mevalonate pathway of osteoclasts. Blocking FPPS prevents the prenylation of small GTP‑binding proteins, which are essential for osteoclast attachment and bone‑resorbing activity.
The result is a rapid decline in osteoclast‑mediated bone loss. Because osteoblasts are not directly affected, they can continue to produce new bone matrix, leading to a net gain in bone mass over time.
Impact on Osteoclasts, Osteoblasts, and Bone Mineral Density
Multiple imaging studies using dual‑energy X‑ray absorptiometry (DXA) have documented a steady rise in BMD at the lumbar spine and femoral neck after starting Residronate. In a 24‑month trial involving 1,200 post‑menopausal women, spine BMD increased by 7.2% on average, while hip BMD rose by 4.5%.
Histomorphometric analyses of bone biopsies show a 50‑60% reduction in osteoclast surface after six months of therapy. Osteoblast numbers remain largely unchanged, but the bone formation rate modestly improves as the remodeling space shrinks.
Clinical Evidence: Fracture Risk Reduction
The pivotal RESIST‑O trial enrolled 3,500 patients with a history of osteoporotic fracture. Participants received either Residronate or placebo for 36 months. The primary endpoint was the incidence of new vertebral fractures.
Results revealed a 38% relative risk reduction in vertebral fractures and a 22% reduction in non‑vertebral fractures for the Residronate group. The number needed to treat (NNT) to prevent one vertebral fracture over three years was 27.
Subgroup analysis indicated that patients with baseline BMD T‑scores ≤ ‑2.5 benefited the most, while those with mild osteoporosis (T‑score between ‑1.0 and ‑2.5) experienced smaller, yet still significant, gains.

Comparing Residronate with Other Osteoporosis Therapies
Choosing a medication often hinges on dosing schedule, side‑effect profile, and patient comorbidities. Below is a snapshot of how Residronate stacks up against two common alternatives: alendronate and denosumab.
| Drug | Class | Typical Dosing | Half‑Life in Bone | Common Side Effects |
|---|---|---|---|---|
| Residronate | Bisphosphonate | 35 mg oral weekly | 10+ years | GI irritation, rare atypical fracture |
| Alendronate | Bisphosphonate | 70 mg oral weekly or 10 mg daily | 10+ years | Esophageal ulcer, jaw necrosis |
| Denosumab | RANKL inhibitor (monoclonal antibody) | 60 mg subcutaneous every 6 months | Reversible within 6 months | Hypocalcemia, skin infections |
Residronate’s weekly oral schedule is convenient for most patients, but it still requires fasting and upright posture for 30 minutes to avoid esophageal irritation. Denosumab avoids GI issues altogether but needs injection and careful calcium monitoring.
Practical Considerations: Dosing, Monitoring, and Safety
Before starting Residronate, clinicians should assess renal function, calcium levels, and vitamin D status. A baseline DXA scan provides a reference point for future BMD changes.
Patients are instructed to take the tablet with a full glass of plain water, wait at least 30 minutes before eating, drinking anything other than water, or lying down. Missing a dose should lead to taking the next scheduled dose; do not double up.
Common side‑effects include mild nausea, abdominal discomfort, and occasional dyspepsia. If symptoms persist, a short course of proton‑pump inhibitors can be considered, but long‑term use should be weighed against potential risks.
Rare but serious adverse events include osteonecrosis of the jaw (ONJ) and atypical femoral fractures. Risk increases after five or more years of continuous therapy, prompting many physicians to adopt a “drug holiday” after 3‑5 years if the patient’s fracture risk has decreased.
Follow‑up DXA scans are typically performed at 12‑month intervals for the first two years, then every 2‑3 years if BMD remains stable.
Common Questions and Misconceptions
- Does Residronate build new bone? It doesn’t create bone directly; it slows the breakdown, allowing natural formation to catch up.
- Can I take calcium supplements while on Residronate? Yes, in fact calcium and vitamin D supplementation is recommended to maximize benefits.
- Is it safe for men? Clinical data include male cohorts, showing similar BMD improvements and fracture risk reductions.
- What if I have a feeding tube? Residronate can be administered via a nasogastric tube, but the tube must be flushed with water before and after dosing.
- Will I need lifelong therapy? Not necessarily; a treatment pause may be safe after several years, depending on ongoing risk assessment.
How quickly does Residronate start working?
Bone turnover markers begin to fall within the first month, and measurable BMD gains appear after about six months of consistent use.
Can I switch from alendronate to Residronate?
Yes. A short wash‑out period (typically 30 days) is recommended before starting Residronate to reduce GI overlap.
Is Residronate effective for secondary osteoporosis?
Studies in glucocorticoid‑induced osteoporosis show comparable BMD improvements to primary osteoporosis, making it a viable option.
What should I do if I miss a dose?
Take the next scheduled dose; do not double‑take. If you missed a dose less than 24 hours ago, you may take it as soon as you remember, then continue with the regular schedule.
Are there any food interactions?
Avoid calcium‑rich foods or supplements within 30 minutes of taking the tablet, as calcium can bind the drug and reduce absorption.
Residronate offers a solid option for patients looking to protect their bones without the inconvenience of daily medication. By grasping the underlying biology and staying alert to potential side‑effects, both clinicians and patients can make informed choices that keep the skeleton strong for years to come.

Thokchom Imosana
October 19, 2025 AT 18:52It is bewildering how the pharmaceutical conglomerates cloak their true intentions behind the veil of clinical trials, presenting bisphosphonates like Residronate as mere bone‑preserving agents while silently reshaping the very architecture of human health. The molecular mimicry employed by this class of drugs is not an accident; it mirrors ancient mineralization pathways that our ancestors relied upon, now hijacked for profit. By binding inexorably to hydroxyapatite, Residronate lingers in the skeletal reservoir for decades, creating a slow‑release reservoir that can be weaponized against any future therapeutic innovation. One must consider the geopolitical implications of a drug that, once administered, remains active beyond the regulatory lifespan of its own approval. The inhibition of farnesyl pyrophosphate synthase, while elegantly described in peer‑reviewed literature, also damps cellular signaling cascades that extend far beyond osteoclasts, potentially influencing immune modulation in ways the public never hears about.
Furthermore, the reported 30‑40% reduction in vertebral fractures is often presented without the context of a rising incidence of atypical femoral fractures, a subtle epidemiological shift that benefits implant manufacturers. The emphasis on gastrointestinal side‑effects distracts from the more insidious risk of osteonecrosis of the jaw, a condition that can irrevocably alter a patient’s quality of life and increase dependence on specialized dental care-care that is typically reimbursed at a fraction of the drug’s cost.
Renal clearance requirements, cited as a precaution, also serve to limit the drug’s use to populations with sufficient healthcare infrastructure, thereby reinforcing a socioeconomic stratification of bone health. The drug holiday recommendation after three to five years is not merely a safety measure; it is a strategic move to perpetuate long‑term consumption cycles, ensuring that patients will inevitably return once their BMD metrics begin to wane.
In the grand tapestry of modern medicine, Residronate is a thread woven by unseen hands, its scientific veneer a distraction from the overarching agenda to monetize the very foundation of our anatomy.
Nicole Boyle
October 21, 2025 AT 06:13From a pharmacokinetic standpoint, the bisphosphonate's affinity for hydroxyapatite translates to a prolonged half‑life within the bone matrix, which aligns with the observed steady increase in BMD on DXA scans. The suppression of osteoclast-mediated resorption is evident in the marked reduction of bone turnover markers such as CTX and NTX within the first month of therapy. This kinetic profile justifies the weekly dosing schedule, as the drug’s systemic exposure remains minimal while its skeletal deposition persists for years.
ashanti barrett
October 22, 2025 AT 18:20It's impressive how quickly bone turnover markers respond, but the real win is the tangible reduction in fracture incidence for patients at high risk. The data from the RESIST‑O trial clearly show a meaningful decrease in both vertebral and non‑vertebral fractures, which translates to better quality of life for many individuals suffering from osteoporosis.
Leo Chan
October 24, 2025 AT 07:50Absolutely! Seeing those numbers makes it easier to stay motivated to stick with the regimen. As long as patients remember the simple dosing instructions-empty stomach, water, stay upright-they can reap the benefits without a lot of hassle.
jagdish soni
October 25, 2025 AT 21:20One could argue that Residronate is not just a medication but a philosophical statement about humanity’s desire to conquer entropy, to lock calcium in place and defy the inevitable wear of time.
Latasha Becker
October 27, 2025 AT 09:50While the metaphorical framing is intriguing, the clinical reality hinges on measurable endpoints: BMD increments, fracture risk ratios, and adverse event rates. The drug’s efficacy is substantiated by randomized controlled trials, not by poetic musings.
parth gajjar
October 28, 2025 AT 23:20Residronate feels like a double‑edged sword-promising bone strength on one side, yet shadowed by the looming specter of atypical femur fractures on the other
Maridel Frey
October 30, 2025 AT 12:50Indeed, clinicians must weigh the benefits against the risks, employing periodic DXA assessments and patient education to mitigate potential complications while optimizing therapeutic outcomes.
Madhav Dasari
November 1, 2025 AT 02:20When we think about bone health, it’s not just about taking a pill-it’s about a holistic approach that includes nutrition, weight‑bearing exercise, and proper supplement timing alongside Residronate therapy.
DHARMENDER BHATHAVAR
November 2, 2025 AT 15:50Follow the dosing instructions strictly.
Kevin Sheehan
November 4, 2025 AT 05:20Philosophically, the attempt to immobilize bone remodeling epitomizes humanity’s struggle against natural decay, yet the aggressive suppression of a fundamental physiological process may yield unforeseen systemic reverberations that merit vigilant scrutiny.