Rhabdomyolysis from Medication Interactions: How Common Drug Combos Cause Muscle Breakdown
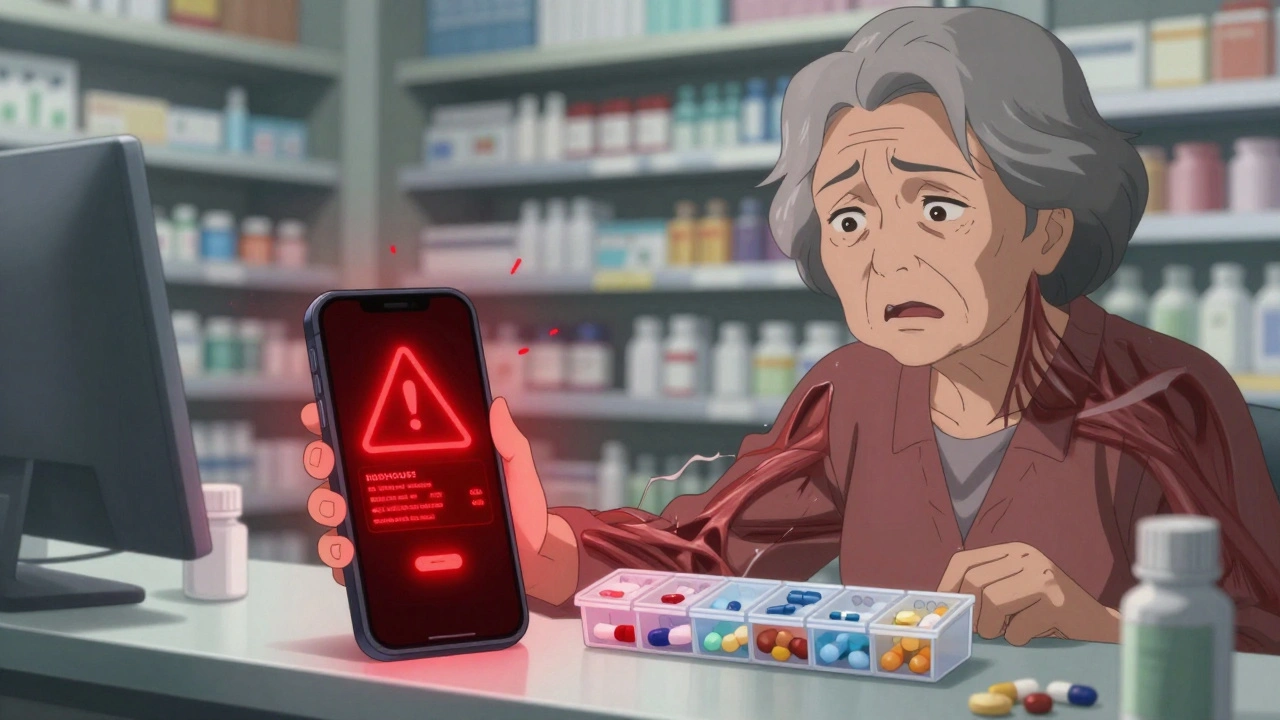
Rhabdomyolysis Medication Interaction Checker
Check if your medications may cause rhabdomyolysis, a serious muscle breakdown condition that can lead to kidney failure. Select your statin and other medications to see the risk level.
No dangerous interaction detected
Your medication combination appears safe. However, always consult with your healthcare provider before making changes to your medication regimen.
DANGEROUS INTERACTION
This combination significantly increases your risk of rhabdomyolysis.
What this means: This combination can cause rapid muscle breakdown (rhabdomyolysis) that may lead to kidney failure. Risk increases by times compared to using the statin alone.
Common symptoms include muscle pain, weakness, dark urine (like cola), and fatigue. If you experience these symptoms, seek immediate medical attention.
What to do: Consult your healthcare provider immediately. This combination may need to be changed or avoided.
MODERATE RISK
This combination may increase your risk of rhabdomyolysis.
What this means: This combination may cause rhabdomyolysis, especially in high-risk individuals such as older adults or those with kidney disease.
What to do: Discuss with your healthcare provider whether alternative medications may be safer for you. Be vigilant for symptoms like muscle pain or dark urine.
Important Notes:
This tool is for informational purposes only and does not replace medical advice. Always consult your healthcare provider about your medication safety.
Rhabdomyolysis can occur rapidly. If you experience muscle pain, weakness, or dark urine after starting a new medication, seek immediate medical attention.
Imagine taking your daily statin for cholesterol, then getting sick with a cold and picking up an antibiotic like clarithromycin. Within days, your muscles ache, your urine turns dark, and you can barely stand. This isn’t just bad luck-it’s rhabdomyolysis, a medical emergency triggered by common drug combinations that many doctors still overlook.
What Exactly Is Rhabdomyolysis?
Rhabdomyolysis happens when muscle cells break down rapidly, spilling their contents into your bloodstream. The most dangerous of these is myoglobin, a protein that can clog your kidneys and cause acute kidney failure. It’s not rare-about 7-10% of all rhabdomyolysis cases come from medications, not trauma or extreme exercise. And it’s getting worse.Most people think of rhabdomyolysis as something that happens to marathon runners or crash victims. But in reality, the biggest driver today is drug interactions. Statins, the most commonly prescribed cholesterol meds, are involved in nearly two-thirds of all medication-related cases. When combined with certain antibiotics, antifungals, or even gout drugs, the risk spikes dramatically.
The Top Drug Combos That Trigger Muscle Breakdown
Some drug pairs are like chemical landmines. Here are the most dangerous combinations, backed by real clinical data:
- Simvastatin + Clarithromycin: This combo increases rhabdomyolysis risk by nearly 19 times. Simvastatin is broken down by the liver enzyme CYP3A4. Clarithromycin shuts that enzyme down, causing simvastatin to build up to toxic levels. One patient reported CK levels hitting 28,500 U/L after just two days on this combo.
- Simvastatin + Gemfibrozil: A 15-20 times higher risk than statin alone. Gemfibrozil doesn’t just inhibit CYP3A4-it also blocks another cleanup pathway, making it a double threat. The FDA has issued multiple warnings about this pairing.
- Colchicine + CYP3A4 Inhibitors: Used for gout, colchicine is fine alone. But when paired with drugs like erythromycin or itraconazole, it causes severe muscle damage in nearly 9% of cases. The European Medicines Agency issued a formal alert in 2021 after reviewing over 1,200 cases.
- Erlotinib + Simvastatin: A cancer drug combined with a cholesterol pill. This mix has caused CK levels over 20,000 U/L in under 72 hours. Oncologists often don’t realize the danger because they’re focused on the cancer, not the statin.
- Propofol (in ICU) + prolonged infusion: Rare but deadly. Propofol can shut down muscle cell energy production, leading to rapid breakdown. Mortality hits 68% when rhabdomyolysis develops.
These aren’t edge cases. They’re repeatable, predictable, and preventable. Yet, studies show that 92% of patients who developed rhabdomyolysis from drug interactions said their provider never warned them.
Who’s at Highest Risk?
It’s not just about the drugs-it’s about who’s taking them.
- Age 65+: Older adults face more than triple the risk. Their kidneys don’t clear drugs as well, and their muscles are more vulnerable.
- Women: They’re 1.7 times more likely than men to develop drug-induced rhabdomyolysis, possibly due to differences in muscle mass and metabolism.
- People with kidney disease: If your eGFR is below 60, your risk jumps 4.5 times. Even mild kidney trouble makes you vulnerable.
- People on five or more medications: Polypharmacy is the silent killer here. Taking five or more drugs increases your risk by over 17 times. That’s not just a stat-it’s a ticking time bomb for many elderly patients.
- Those with the SLCO1B1*5 gene variant: This genetic marker, found in about 15% of Europeans, makes simvastatin 4.5 times more likely to cause muscle damage. Testing for it isn’t routine-but it should be.
The Symptoms Nobody Talks About
Doctors teach the "classic triad": muscle pain, weakness, and dark urine. But here’s the problem-only about half of patients show all three.
More common and misleading signs include:
- Abdominal pain (mimics gallbladder or stomach issues)
- Nausea or vomiting
- Fever without infection
- Decreased urination
- Generalized fatigue that doesn’t improve with rest
One patient on Reddit wrote: "I thought I had the flu. I was in the ER three days later with a CK of 42,000 and dialysis lined up." That’s the pattern. People dismiss it as tiredness or a virus. By the time they get tested, the damage is already underway.
How Doctors Diagnose It
There’s no single test-but creatine kinase (CK) is the gold standard. Normal levels are under 200 U/L. When CK exceeds 1,000 U/L, rhabdomyolysis is likely. In severe cases, it can hit 100,000 U/L or higher.
Doctors also check:
- Myoglobin in urine (dark, cola-colored urine)
- Electrolytes: potassium often spikes (hyperkalemia), calcium drops (hypocalcemia)
- Renal function: creatinine and BUN rise as kidneys struggle
CK levels rise within 12 hours of muscle damage, peak at 24-72 hours, and fall slowly over days. Serial testing is critical. One-time tests can miss the trend.
What Happens in the ER
Time is muscle-and kidney. Treatment starts immediately:
- Stop the offending drug(s): No exceptions. Even if it’s your blood pressure pill or cholesterol med, it must go.
- Aggressive IV fluids: At least 3 liters of saline in the first 6 hours, then 1.5 liters per hour. Goal: urine output of 200-300 mL/hour.
- Urine alkalinization: Sodium bicarbonate is added to IV fluids to keep urine pH above 6.5. This prevents myoglobin from clumping in the kidneys.
- Monitor for complications: High potassium can cause cardiac arrest. Low calcium can trigger seizures. Compartment syndrome (pressure buildup in muscles) may need emergency surgery.
- Dialysis: Needed in up to half of severe cases. If kidneys fail, dialysis buys time until they recover-or doesn’t.
The Cleveland Clinic’s protocol is clear: if CK is above 5,000 U/L, start bicarbonate immediately. Delaying fluids by even a few hours can mean the difference between full recovery and permanent kidney damage.
Recovery and Long-Term Effects
Most people survive-if treated fast. But recovery isn’t simple.
- Without kidney failure: Full muscle recovery takes about 12 weeks on average.
- With dialysis: Recovery can stretch to 28 weeks or longer.
- 43% of survivors still report muscle weakness six months later.
- Some never regain full strength.
And here’s the hidden cost: hospital stays average $28,743 per case. That’s not insurance-it’s out-of-pocket risk for many patients. And with over 27,000 hospitalizations a year in the U.S. alone, this isn’t a niche problem. It’s a systemic failure.

Why This Keeps Happening
Doctors aren’t careless. The problem is complexity.
There are over 200 drugs that interact with CYP3A4. Statins alone come in five types, with different metabolic paths. Simvastatin and lovastatin are high-risk. Atorvastatin is moderate. Pravastatin and rosuvastatin are safer. But most providers don’t know the difference.
Electronic health records rarely flag these interactions clearly. A 2022 study found that 89% of fatal cases involved a CYP3A4 inhibitor-but only 12% of those patients had received a warning from their pharmacy system.
Meanwhile, the FDA and EMA have updated labeling requirements, but those changes don’t always reach frontline prescribers. Patients are left to connect the dots.
What You Can Do
You don’t need to be a doctor to protect yourself.
- Know your meds: Write down every pill you take, including supplements and OTC drugs like ibuprofen or antifungals.
- Ask: "Could this interact with my statin?" Especially if you’re on simvastatin or lovastatin.
- Watch for dark urine: If your pee turns brown or cola-colored after starting a new drug, go to the ER. Don’t wait.
- Request a CK test if you have unexplained muscle pain or weakness after starting a new medication.
- Ask about genetic testing: If you’re on simvastatin and have family history of muscle issues, ask about SLCO1B1 testing.
- Use a drug interaction checker: Apps like Medscape or Epocrates are free. Run your combo before you start a new pill.
One woman told her doctor she felt "off" after adding a new antifungal. He dismissed it. Two days later, she was in the ICU. She survived. But she lost three months of work. She still can’t lift her grandkids.
The Future: Better Alerts, Better Safety
There’s hope. The NIH is funding a $2.4 million project to build real-time drug interaction alerts that actually work. The European Renal Association is testing drugs that protect muscle mitochondria during statin therapy. And the FDA’s Sentinel system is now tracking rhabdomyolysis signals from millions of electronic health records.
But until those systems are fully live, the burden is on you.
Medications save lives. But when they collide, they can destroy them. Rhabdomyolysis isn’t a rare side effect-it’s a preventable emergency. And the best defense isn’t a lab test. It’s awareness.
Can you get rhabdomyolysis from just one medication?
Yes, but it’s rare. Most cases (over 80%) involve drug interactions. Single-drug rhabdomyolysis usually happens with very high doses of statins, especially in elderly patients or those with kidney problems. Some drugs like colchicine, propofol, or certain antivirals can cause it alone-but the risk skyrockets when combined with other meds.
Are all statins equally dangerous?
No. Simvastatin and lovastatin are the riskiest because they’re heavily processed by the CYP3A4 enzyme. Atorvastatin carries moderate risk. Pravastatin and rosuvastatin are much safer because they’re cleared differently-through the kidneys, not the liver. If you’re on a high-risk statin and need a new drug, ask your doctor if switching to pravastatin or rosuvastatin is an option.
How long does it take for rhabdomyolysis to develop after starting a new drug?
Most cases appear within 30 days. Statin-related cases typically show up around 28-30 days after starting or increasing the dose. But with strong interactions-like simvastatin plus clarithromycin-symptoms can hit within 48 hours. If you feel unusual muscle pain or see dark urine after starting a new medication, don’t wait. Get checked.
Is rhabdomyolysis reversible?
Yes-if caught early. Stopping the drug and starting aggressive IV fluids within hours can prevent kidney damage. Many people recover fully. But if kidney failure occurs, recovery takes longer, and some patients never regain full muscle strength. About 44% still report weakness six months later. The key is speed: the sooner you act, the better your outcome.
Should I stop my statin if I’m prescribed an antibiotic?
Don’t stop on your own. But do ask your doctor: "Is this antibiotic safe with my statin?" If you’re on simvastatin or lovastatin, and the antibiotic is clarithromycin, erythromycin, itraconazole, or fluconazole, the answer is likely no. Your doctor may switch your statin to pravastatin or rosuvastatin, or choose a different antibiotic. Never assume it’s safe just because both drugs are commonly prescribed.

Shubham Mathur
December 8, 2025 AT 02:07Bro this is insane I had a cousin on simva + clarithro and he ended up in ICU for 11 days
They didn't even warn him his pharmacist didn't flag it
My aunt took the same combo and her CK hit 38k she still walks with a cane
Why are we still letting this happen
Doctors are so focused on the big stuff they miss the quiet killers
And don't even get me started on how pharmacies ignore these alerts
It's not just statins it's the whole damn system
My mom's on 7 meds and no one ever asked if they interact
We need mandatory interaction checks before any script is filled
Not optional not nice to have mandatory
People are dying because we treat drug safety like an afterthought
And the worst part
It's all preventable
Delaine Kiara
December 9, 2025 AT 05:41OMG I JUST REALIZED I’M ON SIMVASTATIN AND TOOK FLUCONAZOLE LAST WEEK FOR A YEAST INFECTION
MY MUSCLES HAVE BEEN ACHING FOR 3 DAYS
I’M GOING TO THE ER TOMORROW
THANK YOU FOR THIS POST
Noah Raines
December 10, 2025 AT 04:06Same. I was on simva for 5 years with zero issues. Then got azithromycin for bronchitis last month. Now I feel like I got hit by a truck after a 10K run.
CK was 8k. Docs just said 'take a break from the gym.'
Not cool.
And yeah the pharmacy app didn't even blink.
Stacy Tolbert
December 12, 2025 AT 02:05I’m crying reading this. My dad passed last year from this. They said it was 'old age' and 'muscle loss.'
He was on simvastatin and fluconazole for a fungal nail infection.
He told me his legs felt heavy but I thought he was just tired.
He was 71. He never had heart problems. He just wanted to live.
Why didn’t anyone tell us?
Why didn’t anyone stop it?
Katherine Rodgers
December 12, 2025 AT 22:28Oh no not another 'drug interaction' post where everyone acts like they're the first person to discover that mixing meds can be bad
Did you know caffeine can kill you if you take it with MAOIs too?
Maybe we should all just stop taking medicine and eat kale instead
Also your statin isn't 'toxic' it's just metabolized
Stop being dramatic
Sarah Gray
December 14, 2025 AT 14:24It's not the drugs that are dangerous-it's the ignorance of the prescribers. The FDA has issued over 17 safety communications on CYP3A4-mediated interactions since 2018. The fact that this is still happening suggests a systemic failure in continuing medical education.
Furthermore, the notion that 'patients should check their own interactions' is a dangerous abdication of clinical responsibility. Pharmacists are trained to identify these risks. If their systems aren't flagging them, it's not the patient's fault-it's the EHR vendor's.
And while we're at it, the SLCO1B1*5 variant is not a 'gene test'-it's a pharmacogenomic biomarker. Precision medicine isn't optional anymore. It's the standard of care.
Also, propofol-induced rhabdo isn't 'rare'-it's underreported because it's confined to ICUs and rarely makes it into outpatient databases.
Do better.
Brianna Black
December 16, 2025 AT 13:27As someone who works in hospital pharmacy, I see this every single week.
It’s not that doctors are negligent-it’s that the EHR alerts are so loud and useless that they’ve been trained to ignore them.
We get 12 alerts per patient per visit. 11 of them are 'ibuprofen + aspirin = possible GI bleed' (which is true but irrelevant for a 65-year-old on daily baby aspirin).
And then the one alert that matters-simvastatin + clarithromycin-gets buried under 100 'this drug may cause drowsiness' warnings.
We’ve tried redesigning them. We’ve tried color-coding. We’ve tried pop-ups.
Nothing works until you make the high-risk interactions impossible to override.
Like, if the system says 'THIS COMBO CAN KILL YOU,' it should require a second prescriber signature.
It’s not about more tech-it’s about smarter tech.
And yes, I’ve had patients cry in my office because they didn’t know their meds could do this.
We’re not saving lives-we’re just not killing them as fast as we used to.
Ruth Witte
December 17, 2025 AT 15:37THIS IS SO IMPORTANT!! 💪❤️
MY MOM JUST GOT OFF SIMVASTATIN AND NOW SHE CAN WALK AGAIN!!! 🙌
WE SWITCHED TO ROSUVASTATIN AND SHE’S BACK TO GARDENING AND DANCING WITH HER GRANDKIDS!! 🌸💃
PLEASE TELL EVERYONE YOU KNOW!!!
YOU ARE NOT WEAK IF YOU NEED TO CHANGE MEDS!! 💥
YOUR BODY TALKS-LISTEN!!! 🗣️❤️
George Taylor
December 19, 2025 AT 06:12...I'm just gonna say it...
Why are we still talking about this like it's news?
I've seen this exact post on Reddit three times in the last two years.
And every time, someone says 'I didn't know!' and then gets diagnosed.
And then someone else says 'I'm going to the ER.'
And then someone else says 'my dad died.'
And then the cycle repeats.
Nothing changes.
It's like watching a car crash on repeat and nobody puts up a barrier.
Just... stop.
Let the system fix itself.
Or don't.
I'm done.