Risks Associated with Any Medication or Dietary Supplement: What You Need to Know

Most people think if something is labeled "natural," it must be safe. That’s a dangerous myth. Whether it’s a prescription pill, an over-the-counter painkiller, or a bottle of herbal capsules from the health store, every substance you put into your body has the potential to cause harm - sometimes serious, sometimes life-threatening. And the biggest problem? You’re probably not telling your doctor about the supplements you’re taking.
Why Supplements Aren’t Treated Like Medicine
Dietary supplements don’t have to prove they work before they hit the shelves. Under the 1994 Dietary Supplement Health and Education Act (DSHEA), companies can sell vitamins, herbs, amino acids, and other products without FDA approval. The FDA can only step in after someone gets hurt. That means dangerous products can stay on the market for months - even years - before anyone takes them off. This isn’t theoretical. In 2022, the FDA received over 5,000 reports of adverse events linked to supplements. But experts say that’s just the tip of the iceberg. One study estimates that for every reported case, 20 go unreported. That’s why over 23,000 people end up in U.S. emergency rooms every year because of supplements. And it’s not just the exotic ones. Even common multivitamins have caused hospitalizations when taken in high doses or mixed with other drugs.Supplements That Can Kill When Mixed With Medications
The real danger isn’t just the supplement itself - it’s what happens when it meets your prescription. Many supplements interact with medications in ways that are invisible until it’s too late. Take St. John’s wort, a popular herb for mood support. It’s sold as a "natural antidepressant," but it’s not harmless. It can cut the effectiveness of birth control pills by 13-15%, leading to unplanned pregnancies. It can slash cyclosporine levels - a drug used after organ transplants - by half, putting patients at risk of rejection. And when taken with antidepressants like sertraline, it can trigger serotonin syndrome: a condition that causes confusion, rapid heartbeat, high fever, and seizures. One patient in the FDA’s database reported serotonin syndrome after combining St. John’s wort with his antidepressant. He spent three days in the ICU. Then there’s ginkgo biloba, often taken for memory. It thins the blood. When mixed with aspirin, warfarin, or even ibuprofen, it can cause uncontrolled bleeding. A 68-year-old woman in Ohio was hospitalized after combining ginkgo with daily aspirin. She lost so much blood she needed a transfusion. Goldenseal and bitter orange are two other hidden threats. Goldenseal interferes with how the liver breaks down dozens of medications, including statins, blood pressure drugs, and even some cancer treatments. Bitter orange - found in weight-loss supplements - can spike blood pressure and trigger irregular heart rhythms. One Reddit user reported heart palpitations and insomnia after taking ashwagandha with his blood pressure medication. He didn’t realize the supplement could interfere with his prescription.Vitamins Can Be Toxic Too
People assume vitamins are harmless because they’re essential for life. But more isn’t better. Too much of the wrong vitamin can damage your organs. Vitamin A toxicity happens when people take more than 10,000 IU daily over time. Symptoms include dry skin, hair loss, liver damage, and increased pressure in the brain - which can cause blurred vision and headaches. One woman in her 50s started taking 25,000 IU daily for "immune support" and ended up with liver scarring. Vitamin D is another silent danger. High doses - especially over 300,000 IU per month - can cause hypercalcemia: too much calcium in the blood. That leads to nausea, vomiting, kidney stones, and even heart rhythm problems. In older adults, it increases the risk of falls and fractures by 15-20%. Vitamin E at doses over 400 IU daily raises the risk of hemorrhagic stroke by 10%. That’s not a small increase. It’s enough to make doctors warn against high-dose use, especially in people on blood thinners. Vitamin K is even trickier. It directly opposes warfarin, a common blood thinner. Taking even a small amount of vitamin K - say, from a green supplement or a multivitamin - can make warfarin useless. One patient’s INR (a blood clotting test) dropped from 3.2 to 1.1 in just three days after starting a vitamin K supplement. He had a stroke two weeks later.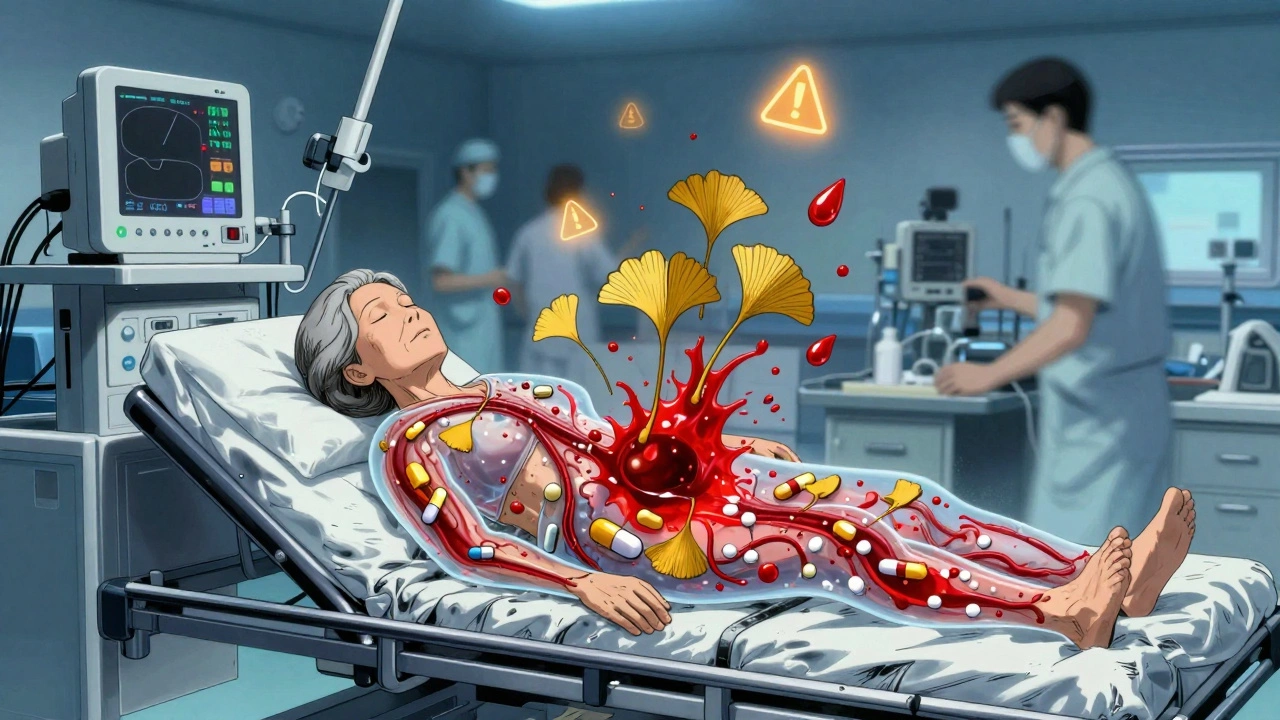
Supplements and Cancer Treatment: A Dangerous Mix
If you’re undergoing cancer treatment, the risks multiply. Antioxidants like vitamins C and E are often marketed as "protective," but they can interfere with chemotherapy and radiation. Studies show they may reduce treatment effectiveness by 25-30% in certain cancers. Radiation oncologists at Memorial Sloan Kettering have seen patients develop severe skin burns during radiation because they were taking vitamin E supplements. One patient had to pause treatment for three weeks while his skin healed. The American Cancer Society’s advice is clear: avoid all supplements during cancer treatment unless your oncologist specifically says it’s safe. Why? Because supplements aren’t tested alongside chemotherapy drugs. No one knows how they’ll react. And when they do react, it’s often too late.Who’s Most at Risk?
Older adults are the most vulnerable. Many take multiple medications - five, six, or more - and add supplements on top. The average 70-year-old might be on blood pressure medicine, a statin, a blood thinner, and a joint supplement. Add in a multivitamin, melatonin, and turmeric for "inflammation," and you’ve got a chemical cocktail with unpredictable effects. People with liver or kidney disease are also at higher risk. Their bodies can’t clear toxins as efficiently. Green tea extract, for example, has been linked to over 20% of supplement-related liver injuries. That’s more than any other herb. And then there’s the online market. Nearly half of all supplement-related adverse events come from products bought online - especially from sites outside the U.S. These products often contain hidden ingredients: stimulants, steroids, or even prescription drugs like sildenafil (Viagra) or amphetamines. The FDA has found weight-loss supplements laced with banned substances. One product labeled "natural fat burner" contained a powerful stimulant linked to heart attacks.
What You Can Do to Stay Safe
The good news? Most of these risks are preventable. 1. Tell your doctor everything. Not just prescriptions. Not just the big-name supplements. Tell them about the ashwagandha you take for stress, the fish oil you swallow for your heart, the magnesium you chew before bed. Doctors can’t protect you if they don’t know what you’re taking. Only 33% of people report supplement use to their providers. That’s a huge gap. 2. Keep a written list. Update it every time you start or stop something. Use the NIH’s free "My Dietary Supplement and Medicine Record" tool. It’s simple, printable, and used by over 1,200 clinics. 3. Avoid supplements during surgery or cancer treatment. Unless your surgeon or oncologist says it’s okay, stop everything two weeks before surgery. Many herbs increase bleeding risk. Some interfere with anesthesia. 4. Be skeptical of "miracle" claims. If a product promises "instant energy," "detox," or "cures arthritis," walk away. Real supplements don’t work that way. And if the label doesn’t list all ingredients - or if it says "proprietary blend" - that’s a red flag. You have no idea what you’re getting. 5. Report bad reactions. If you feel sick after taking something, stop it. Call your doctor. And report it to the FDA through MedWatch Online. In 2022, they received over 18,000 supplement reports. Every one helps them spot patterns and protect others.The Bottom Line
Medications and supplements aren’t harmless. They’re both powerful. Both can save lives. Both can end them. The difference? Medications come with warnings, dosage instructions, and clinical data. Supplements? Often, they come with a pretty label and a promise. The safest approach isn’t to avoid all supplements. It’s to treat them like medicine. Ask questions. Check for interactions. Talk to your doctor. And never assume "natural" means safe.Can dietary supplements really interact with prescription drugs?
Yes, and these interactions can be dangerous. For example, St. John’s wort can reduce the effectiveness of birth control pills, antidepressants, and transplant medications. Ginkgo biloba and fish oil can increase bleeding risk when taken with warfarin or aspirin. Even common vitamins like vitamin K can make blood thinners like warfarin ineffective. These aren’t rare cases - they’re well-documented in clinical studies and FDA reports.
Are natural supplements safer than prescription drugs?
No. The word "natural" doesn’t mean safe. Many plant-based supplements contain potent chemicals that affect your body just like drugs. Bitter orange can raise blood pressure. Green tea extract can damage your liver. Even vitamin A and D can become toxic at high doses. Prescription drugs go through years of testing. Supplements don’t. That makes them riskier in many ways.
Why doesn’t the FDA ban dangerous supplements faster?
Under current law, the FDA can’t ban a supplement unless it proves it’s unsafe after people are already harmed. Manufacturers don’t need to prove safety before selling. So dangerous products can stay on shelves for years while the FDA gathers evidence. Since 1994, only 12 ingredients have been banned. Meanwhile, over 85,000 supplement products are on the market.
What supplements should cancer patients avoid?
Cancer patients should avoid all supplements unless approved by their oncologist. Antioxidants like vitamins C and E may reduce chemotherapy effectiveness by 25-30%. Some herbs interfere with how the body processes drugs. Radiation patients have reported severe skin burns from vitamin E. The American Cancer Society recommends stopping all supplements during treatment to avoid unknown risks.
How can I check if my supplement is safe to take with my meds?
Talk to your pharmacist or doctor. Bring your full list - including dosages and brands. You can also check the NIH’s LiverTox database for liver-related risks, or the FDA’s Dietary Supplement Ingredient Advisory List for known dangerous ingredients like bitter orange and yohimbe. Never rely on online forums or store clerks for medical advice.
Is it safe to buy supplements online?
It’s risky. Nearly half of all supplement-related adverse events come from online purchases, especially from international sellers. Many products contain hidden drugs, heavy metals, or unlisted stimulants. A supplement labeled "turmeric" might contain undeclared steroids or banned weight-loss agents. Stick to trusted brands with third-party testing (like USP or NSF) - and even then, talk to your doctor first.
What should I do if I think a supplement made me sick?
Stop taking it immediately. Contact your doctor or go to the ER if you have severe symptoms like chest pain, trouble breathing, or bleeding. Then report it to the FDA through MedWatch Online. Your report helps the agency identify dangerous products and protect others. Don’t assume it’s just a coincidence - your experience could prevent someone else’s hospitalization.

Desmond Khoo
December 7, 2025 AT 06:57Louis Llaine
December 7, 2025 AT 23:34Jane Quitain
December 9, 2025 AT 22:49Ernie Blevins
December 11, 2025 AT 14:22Nancy Carlsen
December 13, 2025 AT 07:11Ted Rosenwasser
December 13, 2025 AT 07:58Kyle Oksten
December 15, 2025 AT 06:37Sam Mathew Cheriyan
December 16, 2025 AT 16:08Olivia Hand
December 17, 2025 AT 13:24Ashley Farmer
December 17, 2025 AT 19:39Jennifer Anderson
December 19, 2025 AT 10:42Sadie Nastor
December 20, 2025 AT 18:27Sangram Lavte
December 21, 2025 AT 17:45Oliver Damon
December 21, 2025 AT 21:45