Spinal Cord Injury: Understanding Function Loss, Rehabilitation, and Assistive Devices

When a spinal cord injury happens, it doesn’t just break bones-it breaks the connection between your brain and your body. The severity of what you lose depends on where the injury sits and how complete it is. Some people lose movement in their legs. Others can’t feel their hands or control their bladder. For many, the shock isn’t just the injury itself-it’s realizing how much daily life changes overnight.
What Happens When the Spinal Cord Is Damaged
The spinal cord is your body’s main communication line. Signals from your brain travel down it to tell your muscles when to move, your organs when to function, and your skin when to feel touch or pain. When it’s injured, those signals get blocked. The higher the injury, the more functions are affected.A C1-C4 injury can leave someone unable to breathe on their own, requiring a ventilator. A T12 injury might mean losing leg movement but keeping full arm function. Incomplete injuries-where some signals still get through-offer more hope for recovery. Complete injuries mean no signals pass below the injury site. About 302,000 people in the U.S. are living with spinal cord injuries right now, with 17,810 new cases every year. Motor vehicle crashes cause nearly 40% of them. Falls are close behind, especially for people over 65.
What you lose isn’t just mobility. Autonomic functions like blood pressure control, temperature regulation, bowel and bladder control, and even sexual function can be disrupted. Many people don’t realize how much daily life depends on these invisible systems until they stop working.
Rehabilitation Starts the Day You’re Stabilized
Rehab doesn’t wait until you’re ready. It starts within 24 to 72 hours after your injury is medically stable. That’s when therapists begin passive range-of-motion exercises-moving your limbs for you-to prevent joints from stiffening and muscles from shrinking. If you’re in a flaccid state, they do this once a day. If spasticity kicks in, they do it two or three times daily.Therapy isn’t just stretching. It’s breathing exercises to prevent pneumonia, especially for high cervical injuries. It’s learning how to shift your weight to avoid pressure sores. It’s training your body to handle changes in blood pressure when you sit up. At top centers like Mayo Clinic or Spaulding Rehabilitation, you’ll get at least three hours of therapy, five days a week, from a team that includes physical therapists, occupational therapists, nurses, psychologists, and social workers.
For incomplete injuries, the first year is critical. Studies show people can regain 80 to 90% of their functional potential during this time. That means learning to stand, take steps with support, or use their hands again. For complete injuries, progress is slower. Only 1 to 3% of complete paraplegics regain walking ability. But even small gains-like better sitting balance or being able to push a manual wheelchair-can change everything.
How Assistive Devices Restore Independence
Assistive devices aren’t just tools-they’re lifelines. A wheelchair isn’t just a chair; it’s your legs. But not all wheelchairs are the same. A custom seating system with pressure-relieving cushions can prevent lifelong sores. A power wheelchair with tilt and recline functions gives you control over your posture and comfort. Medicare covers 80% of basic wheelchair costs, but the rest? That’s $1,200 to $3,500 out of pocket for specialized features.For those with arm function, hand-controlled joysticks or sip-and-puff systems let you move independently. For those with no hand use, voice-controlled wheelchairs are becoming more common. But even the best device fails without proper training. A bad transfer from bed to chair can cause shoulder injuries in caregivers 32% of the time. That’s why therapists spend hours teaching safe transfers, using sliding boards and proper body mechanics.
Then there are the high-tech tools. Functional Electrical Stimulation (FES) bikes use mild electrical pulses to make paralyzed muscles contract, cycling your legs. People with T6 injuries report keeping muscle mass and improving heart health-peak oxygen use goes up 14.3% with FES cycling, compared to just 5.2% with regular arm cycling. But a home FES unit costs $5,000. Insurance rarely covers it.
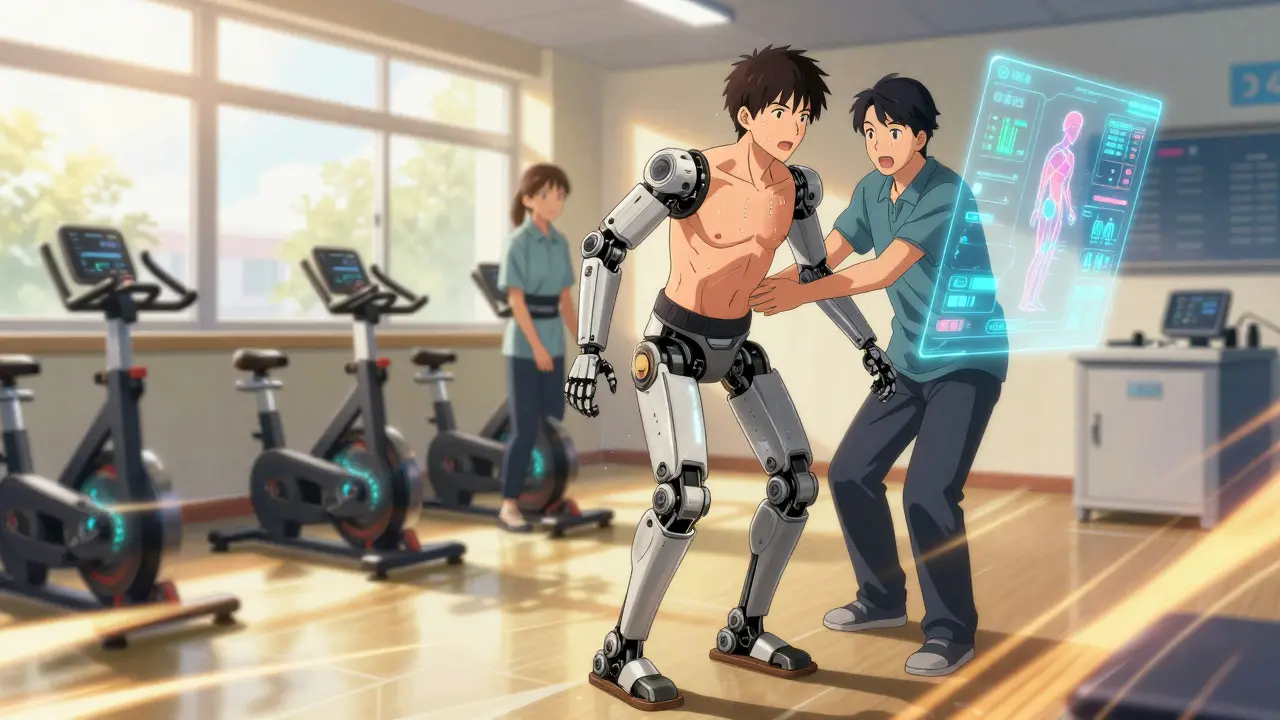
Robotic exoskeletons like Ekso and ReWalk let people with paraplegia stand and take steps. One Reddit user said it gave him his first steps in three years. But each session lasts only 25 to 45 minutes because it’s exhausting. And you need two or three therapists to help you into it safely. These machines cost over $100,000. Most rehab centers have one or two. You don’t get to take one home.
Managing the Hidden Challenges
The biggest struggles aren’t always the ones you see. Neurogenic bladder and bowel take up 45 to 90 minutes every day. You have to catheterize, follow strict schedules, and watch for infections. Spasticity-uncontrolled muscle tightening-affects 65 to 78% of people with SCI. It can lock your joints, cause pain, and make transfers impossible.Doctors manage it with a mix of oral meds like baclofen, targeted Botox injections, and stretching. At Mayo Clinic, 78% of patients see a 40 to 60% drop in spasticity scores with this approach. But it’s not one-size-fits-all. What works for one person might make another feel worse.
Respiratory issues are another silent killer. High cervical injuries weaken coughing. That’s why therapists teach assisted coughing, percussion (tapping on the chest), and incentive spirometry. These techniques cut pneumonia risk by 65%. Yet many patients skip them because they’re tiring or embarrassing.
Technology Is Changing the Game-But Not Everyone Can Access It
The field is moving fast. In 2022, the FDA approved the first fully implantable diaphragm pacing system. For people with C3-C5 injuries, it cuts ventilator use by 74%. That’s life-changing. At Columbia University, researchers developed the Tethered Pelvic Assist Device (TPAD), which helps with balance training during walking rehab. AI-driven therapy plans are now used by 65% of top rehab centers, adjusting workouts in real time based on your progress.But here’s the problem: most of these breakthroughs are still in research or limited to elite centers. Only 32% of general hospitals offer full SCI rehab programs. And even at top facilities, insurance won’t cover everything. Medicare pays only 83% of actual rehab costs. Many patients quit home exercises after six months because no one checks in on them. A survey found 68% stop because they feel alone and unmotivated.
Peer support makes a difference. At Spaulding, 82% of patients say talking to someone who’s been through it improved their mental recovery more than any therapy. That’s not a gadget. That’s human connection.

What Recovery Really Looks Like
Recovery isn’t about walking again. For most, it’s about living well with what you have. It’s learning to dress yourself with adaptive clothing. It’s using voice commands to turn on lights. It’s finding a wheelchair that doesn’t hurt your back. It’s knowing when to ask for help-and when to push through the pain.People who stay active in rehab, who build routines, who connect with others who’ve been there, are the ones who thrive. They don’t necessarily get back what they lost. But they build a new life-one that’s full, meaningful, and under their control.
The road is long. The costs are high. The system isn’t perfect. But progress is real. And for every person who stands in an exoskeleton for the first time, or breathes without a machine, or pushes their wheelchair across a park alone-it’s proof that function doesn’t have to mean what it used to. It can mean something new. Something powerful.
Can you walk again after a spinal cord injury?
It depends on whether the injury is complete or incomplete. About 59% of people with incomplete injuries regain some walking ability, often with assistive devices like walkers or exoskeletons. Only 1 to 3% of those with complete paraplegia regain walking function. Even if you don’t walk, therapy can improve balance, strength, and endurance, making daily life easier.
How long does spinal cord injury rehab last?
Rehab starts immediately after medical stabilization and usually lasts 6 to 12 weeks in an inpatient setting. After that, outpatient therapy continues for months or years. The first year is the most critical for recovery, especially for incomplete injuries. Many people keep doing home exercises and periodic therapy for life to maintain function and prevent complications.
Are robotic exoskeletons worth it for SCI rehab?
They offer real benefits-improved circulation, muscle tone, and psychological boost from standing and stepping. But they’re expensive, require multiple therapists to operate, and sessions are limited to 30-45 minutes. Most people use them in rehab centers, not at home. Long-term outcomes beyond six months are still being studied. For now, they’re a powerful tool, but not a cure.
What’s the biggest challenge after spinal cord injury?
It’s not mobility-it’s managing daily systems like bladder and bowel care, spasticity, and pressure sores. These tasks take hours every day and require strict routines. Many people struggle with motivation, isolation, and lack of follow-up care. Peer support and consistent therapy are key to staying on track.
Does insurance cover spinal cord injury rehab and devices?
Medicare and private insurance cover inpatient rehab and basic wheelchairs, but often leave big gaps. For example, Medicare pays 80% of wheelchair costs after your deductible, leaving $1,200-$3,500 out of pocket for custom seating. FES bikes, exoskeletons, and home modifications are rarely covered. Many patients pay for these themselves or rely on nonprofit aid.
Can spinal cord injury be reversed?
Currently, there’s no cure that fully reverses spinal cord damage. But research is advancing quickly. Implantable diaphragm pacers, brain-computer interfaces, and nerve regeneration therapies are showing promise in trials. While full recovery isn’t possible yet, many people regain significant function through intensive rehab and technology.
What Comes Next
If you or someone you know is facing a spinal cord injury, the first step is finding a certified SCI Model System center. These are the only facilities that meet the highest standards for care, research, and outcomes. Ask your doctor for a referral. Don’t settle for a general rehab unit if you can get specialized care.Connect with support groups-online or in person. You’re not alone. And keep pushing for what you need: better equipment, better coverage, better care. Progress isn’t always fast, but it’s possible. And every small win-standing for a minute, transferring without help, sleeping through the night-adds up to a life lived on your terms.

Stephen Tulloch
January 17, 2026 AT 04:20Bro. I saw a guy in a ReWalk at the mall last week. He was just... rolling through the food court like a boss. No cane, no crutches. Just pure electric confidence. 😎 The way he nodded at the kids staring? Chef’s kiss. This isn’t about walking again-it’s about owning the damn wheelchair like it’s a Tesla.
Joie Cregin
January 17, 2026 AT 20:49That moment when someone says ‘you’ll never walk again’ and then you’re standing in an exoskeleton, laughing while your therapist nearly falls over trying to catch you? That’s the real win. Not the machine. Not the tech. It’s the look on your mom’s face when she sees you stand up for the first time in years. ❤️
Melodie Lesesne
January 18, 2026 AT 03:14I work in rehab and I see this every day. People think recovery is about milestones, but it’s really about the tiny stuff: finally being able to reach the remote, not needing help to scratch an itch, or choosing your own clothes. Those are the victories that last. And yeah, the FES bike? Life-changing. Even if it costs more than my car.
Corey Sawchuk
January 19, 2026 AT 23:51Been there. Spinal injury at 22. Now 38. Still use a chair. Still catheterize. Still hate spasticity. But I ride bikes, travel solo, and taught myself to cook with adaptive tools. Rehab doesn’t fix you. It teaches you how to be you again. Just different. No big drama. Just life.
Samyak Shertok
January 20, 2026 AT 06:19Oh wow so we’re all supposed to be impressed that some rich guy in a $100K robot can stand up for 45 minutes? Meanwhile, the guy in Ohio can’t afford a decent cushion and his pressure sores are getting infected. This isn’t progress. It’s a luxury ad disguised as medicine. 🤡
Bianca Leonhardt
January 21, 2026 AT 19:01Let’s be real. Most people who get spinal injuries are either dumb enough to not wear a seatbelt or old enough to trip on a rug. Stop romanticizing it. Rehab is expensive because you made bad choices. Now deal with it.
Travis Craw
January 21, 2026 AT 19:20u/6912 kinda has a point tho. I mean yeah the tech is cool but like… why does it take 3 therapists just to get someone into a robot? And why can’t you take one home? Feels like they’re selling hope but not the tools to keep it. Also… my cousin’s chair broke and insurance said ‘sorry not covered’
Nicholas Gabriel
January 22, 2026 AT 11:51Everyone’s talking about tech, but the real hero here is the peer support. The person who’s been there, who texts you at 2 a.m. because you’re crying over a catheter bag, who says ‘I’ve been there, it gets better’-that’s the stuff that keeps people alive. No machine does that. No insurance covers that. But it’s priceless.
swarnima singh
January 23, 2026 AT 09:10you think this is bad? wait till you find out the government is using spinal injury patients as test subjects for mind-control tech. they implant chips to monitor your emotions. that’s why they push exoskeletons so hard-they’re tracking your brainwaves. they want to know how much pain you feel. they’re coming for you next.
Isabella Reid
January 24, 2026 AT 03:01I’m from India and I saw a rehab center in Pune that uses recycled wheelchair parts and community volunteers. No fancy tech. No $100K robots. Just people showing up. And guess what? People are walking. Not with machines-with each other. Maybe the real breakthrough isn’t in labs. Maybe it’s in love.
Jody Fahrenkrug
January 24, 2026 AT 16:32My dad had a T12 injury. He didn’t walk again. But he learned to garden in his chair. Grew tomatoes bigger than my head. Said the soil reminded him he still had control. Sometimes the best rehab isn’t in a clinic. It’s in your backyard.
kanchan tiwari
January 26, 2026 AT 09:10they’re lying to you. the real reason they don’t give you the exoskeleton is because if you could walk, you’d go back to work. and then the insurance companies would have to pay for your salary. they want you stuck. they want you dependent. this is all a scam. the government and pharma are in cahoots. they don’t want you healed. they want you hooked.
Bobbi-Marie Nova
January 27, 2026 AT 01:51so like… the FES bike costs $5k and insurance says no? cool. i’ll just buy one and leave it in the park for anyone who needs it. free community bike for paralyzed legs. someone’s gotta start the revolution. also, i made a playlist called ‘Legs That Don’t Work But Hearts That Do’
Allen Davidson
January 27, 2026 AT 11:17Look. I’ve been a PT for 18 years. I’ve seen people cry because they can’t hold their coffee. I’ve seen people cry because they stood up in an exoskeleton. Both matter. The system’s broken? Yeah. But don’t give up on it. Push for coverage. Demand better equipment. Find your tribe. And never, ever let someone tell you your life is over. It’s just… rewritten.
john Mccoskey
January 28, 2026 AT 06:39It’s fascinating how society romanticizes the ‘triumphant spirit’ narrative while ignoring the systemic collapse that leaves people with no access to basic care. The $100,000 exoskeleton is not a miracle-it’s a symptom of a healthcare system that commodifies rehabilitation while denying it to the majority. The fact that 68% of patients discontinue home therapy due to isolation isn’t a personal failure-it’s a policy failure. We’ve turned human dignity into a premium subscription service. And the worst part? We’ve normalized it.